Anichstraße 35
6020 Innsbruck
Fax: +43 50504 22758
Email: radiologie@i-med.ac.at
Website: https://radiologie.tirol-kliniken.at/page.cfm?vpath=radiologie
Research Branch (ÖSTAT Classification)
302010, 302013, 302043, 302044, 302048, 302053, 302055, 302070, 302071, 302074, 302075, 302079
Keywords
artificial intelligence, dose management, DTI, dual-energy-CT, fMRI, High-field MRI, interventional neuroradiology, MR-spectroscopy, multimodal imaging, and quantitative MR-imaging
Research Focus
- Ultrasound (elastography, musculoskelettal, peripheral nerves, ultrasound guided interventions)
- Multiparametric imaging of prostatic cancer
- MRI (quantification of fat/iron; cardiac MRI; spectrosopy of myocardium; musculo Skelettal MRI including stress MRI of the hip and knee, MR mammography)
- Mikro CT
- Cardiac CT
- Dual Energy CT
- Emergency Radiology, trauma, sports injury
- Interventional Radiology (endovascular/oncology)
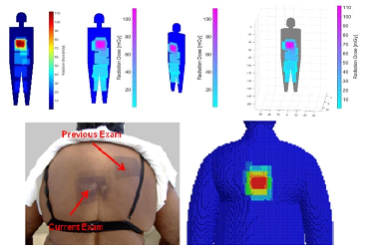
- Real time dose monitoring of patients
- Diagnosis and treatment of HCC (stereotactic RFA, TACE, SIRT)
- Digital imaging/PACS/postprocessing of imaging data, artificial intelligence
- Clinical trials
General Facts
For clinical routine and research, the department is equipped with state-of-the-art imaging systems: 7 CT scanners (2 dual-source/64-slice/40-slice [sliding gantry]), 5 MRI scanners (2x 3T, 3x 1.5T), 2 PET-CT scanners (in cooperation with the Department of Nuclear Medicine), 3 angiography suites (1 biplane) and 15 high-end ultrasound systems. One sliding gantry CT operates in an imaging suite dedicated to stereotaxis and CT-guided procedures. The department has operated fully digitally since 1999, using a comprehensive imaging archive (PACS).
There are 69 staff members, including 31 residents (radiologists in training).
The Experimental Radiology section (https://radiologie.tirol-kliniken.at/page.cfm?vpath=gemeinsame-einrichtungen/exprad) is staffed by 8 physicists/mathematicians with different areas of interest: MRI, MRS, image data processing, radiation protection, deep learning and computer applications.
The department houses research facilities for animals (high-resolution RF coils for MRI, access to PET imaging). Large animals can be imaged on clinical CT and MR scanners. The core facility of Micro-CT (https://radiologie.tirol-kliniken.at/page.cfm?vpath=radiologie/forschung/micro-ct) is equipped with 2 micro-CT scanners, which are operated in cooperation with the Department of Orthopaedics and Traumatology. Both scanners can be used for high-resolution imaging of small animals and one can also be used for high-resolution scanning of extremities, to evaluate patient bone density.
Our research projects are mostly interdisciplinary and clinically oriented. We focus on rapid translation of research results into clinical practice. The two departments have a long-standing PhD programme (Image-Guided Diagnosis & Therapy) and a clinical PhD programme (Clinical Imaging Science). 2021 a FWF grant for the “Image Guided Diagnosis and Therapy” programme (DOC 110-B) was awarded. Within this programme together with the Departments of Nuclear Medicine, ENT, Radiation Therapy and Onkology and Medical Physics the research expertise was enlarged by mathematics, computer science and engineering including partners from the University of Innsbruck LFU (Applied Mathematics and Computer Science) and from the Tyrolean Private University UMIT (Biomedical Engineering).
Research
CT imaging
Gerlig Widmann
a) Head and Neck imaging
- Use of AI for classification of cervical lymph nodes in head and neck cancer
- Frequency an consequences of cervical lymph node overstaging in head and neck carcinoma
b) Thoracic imaging
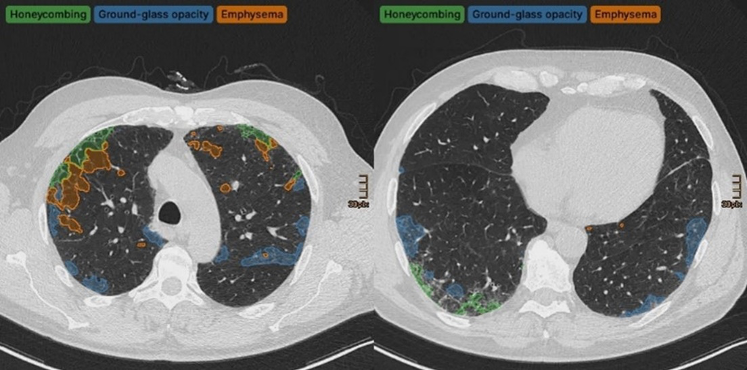
- Quantification of lung injury 1 year after COVID-19 pneumonia.
- Evaluation of AI-based software for lung nodule detection, coronary calcium evaluation, measurement of aortic diameters, emphysema quantification and pneumonia quantification
- Deep learning-based texture analysis and quantification in interstitial lung disease
c) Abdominal imaging
- Dual Energy CT based evaluation of diffuse liver disease and HCC: fibrosis and fat quantification
- Dual Energy CT based quantification of iron content in liver
- Structured reporting as a basis for tumor registry for radiomics research
d) Low dose imaging
- Identification and characterization of patients being exposed to computed-tomography associated radiation-doses above 100 mSv.
- Development of an ALADA reference quality approach in craniofacial trauma CT
- Clinical verification of an ALADA protocol in craniofacial trauma
- Prediction of ALADA Doses for Implant Site Analysis Using Slope of Hounsfield Units- external collaboration with King Saud University
Experimental Radiology
a) Image Processing
Wolfgang Recheis
Image processing and analysis, including rapid prototyping based on radiological data, represent core interests and tasks, including multidimensional visualisation, the quantification of disease patterns based on texture analysis, shape analysis and others. Moreover, our new micro-CT core facility allows depiction of structures on μm scale in all three spatial dimensions.

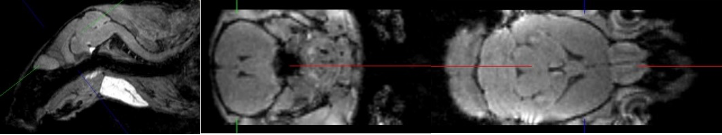
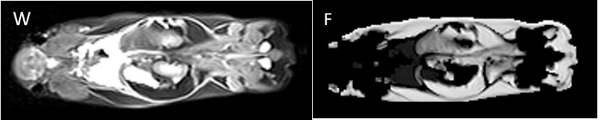
Small Animal MRI
Christian Kremser
In addition to clinically oriented projects, the Department of Radiology conducts experimental MR examinations on various animal models and specimens. Over the years, coil setup and imaging sequences have been optimised accordingly. Study topics include: mouse spinal cord imaging after shock wave treatment to promote spinal cord repair; volumetry of mouse myocardium to quantify fibrotic changes after constriction of the aorta and pulmonary artery; volumetry of the mouse brain to quantify fixation shrinkage; pulse wave velocity imaging in rabbits to evaluate aortic plaques; volumetric quantification of subcutaneous and visceral fat in mice on different diets; detection of intervertebral disc herniation in knockout mice.
MedCorpInn– Retrospective Intersectional Corpuslinguistic Analysis of Radiological and Medical Reports of Medical University of Innsbruck
Claudia Posch and Karoline Irschara (University of Innsbruck), Leonhard Gruber and Stephanie Mangesius (Medical University of Innsbruck)
This project is compiling a large linguistic corpus (digitalised data collection) of radiology reports and medical reports, in order to conduct corpus and discourse linguistic as well as gender medicine research. After standardisation, automated data processing and anonymisation, the radiology corpus contains over 5 million anonymised radiology reports, which can be queried using corpus linguistic and NLP tools. With respect to linguistic patterns and differences, this unique data set can be used e.g. to study whether differences in language use are connected with social and demographic factors.
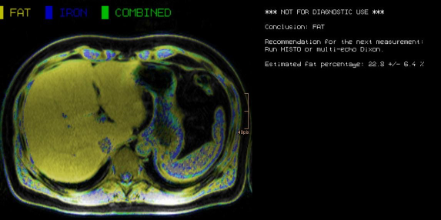
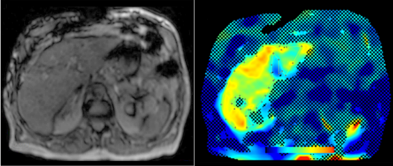
Abdominal MR Imaging
Michaela Plaikner, Benjamin Henninger, Christian Kremser
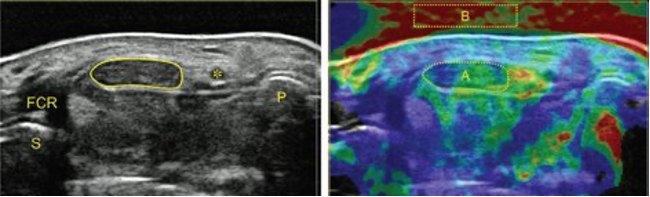
Morphological and functional MRI in all-organ systems development of novel MRI applications and MR sequences. Examples of research projects: fat, iron or combined disease; influence of iron on the evaluation of liver fat (Fig. 5).
a) MRI for the evaluation of diffuse liver disease:
evaluation of different MRI methods (relaxometry, chemical shift imaging, multi-echo approach, Dixon screening), in order to detect diffuse liver disease (fat, iron or combined disease); influence of iron on the evaluation of liver fat (Fig.6).
b) MR-Elastography (MRE)
MRE is increasingly used in hepatic MRI to detect and classify fibrosis in the early stages before morphological changes have occurred. In our department, MRE is already integrated into the routine hepatic MRI protocol and used for various research projects.
Cardiovascular MR Imaging
Agnes Mayr, Christian Kremser, Paulina Poskaite, Mathias Pamminger, Felix Troger, Matthias Schwab in cooperation with the Department of Cardiology
a) STEMI CMR: CMR Parameters of Myocardial Tissue Damage in ST-Elevation Myocardial Infarction (STEMI).
Since 2005, almost 900 patients have been examined under a comprehensive cardiac MRI (CMR) protocol within the first week as well as 4 months, 12 months and 10 years after acute STEMI. In more than 60 internal original papers, CMR myocardial infarction severity markers were assessed and the effects of CMR on optimised risk assessment shortly after STEMI were evaluated.
b) TAVI CMR: CMR to Guide Transcatheter Aortic Valve Implantation (TAVI).
This ongoing randomised study investigates the non-inferiority of TAVI CMR to TAVI CT for the first time, with regard to efficacy and safety end-points in the guidance for TAVI evaluation.
c) 4D Phase Contrast Flow Measurements
- Patients with different grades of aortic valve stenosis: comparison of 4D flow-assessed stenosis severity with 3D echocardiography and invasive measurements.
- Patients with cryptogenic stroke: recording turbulent kinetic energy, changes in flow patterns and regional wall stresses as well as occurrence of a vortex-shaped flow along the thoracic aortic wall, in order to optimise the elucidation of potential cardioembolic sources.
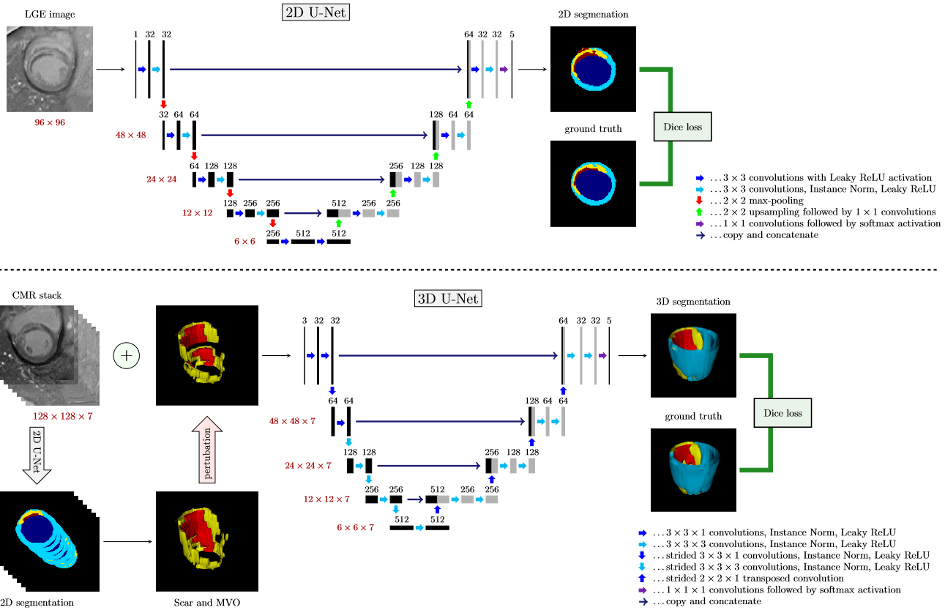
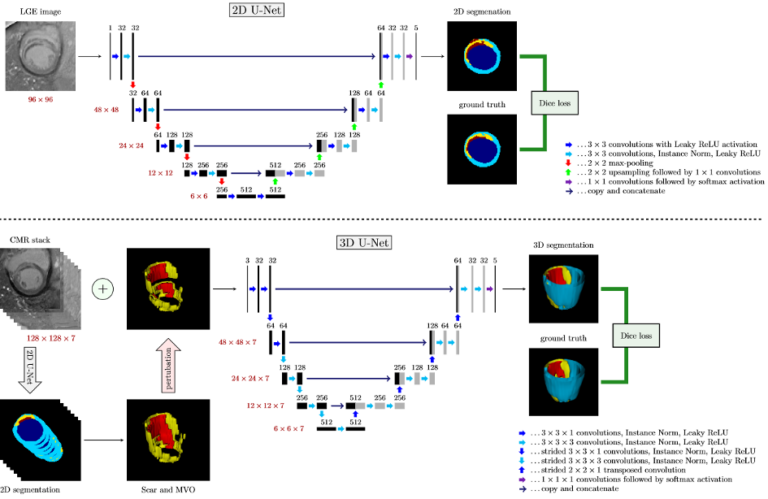
volumes as well as the possibly pertubated segmentation masks for scar and MVO provided by the pre-trained 2D CNN.
d) Deep learning based automatic scar segmentation on late enhancement contrast enhanced MR
This ongoing project aims to develop a fully automatic framework to process 3D cardiac MR datasets for quantification of infarct scars. First results have already achieved results which outperform published state-of-the-art methods.
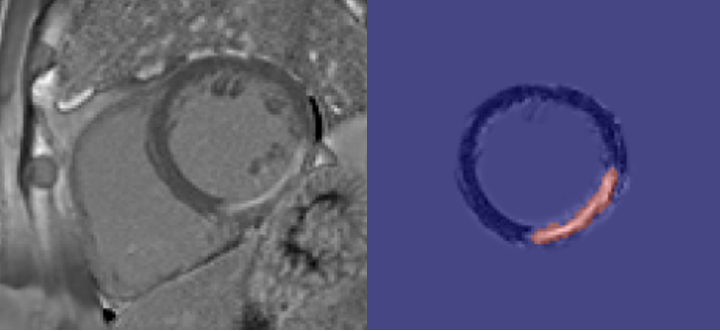
e) Error correcting 2D-3D cascaded network for myocardial scar segmentation on LGE CMR images
In this work, we develop a cascaded framework of two-dimensional and three-dimensional convolutional neural networks that should enable to calculate the extent of myocardial infarction in a fully automated way.
Musculoskeletal Imaging
Andrea S. Klauser et al., Multicentre collaboration for indication in MSK imaging and interventions
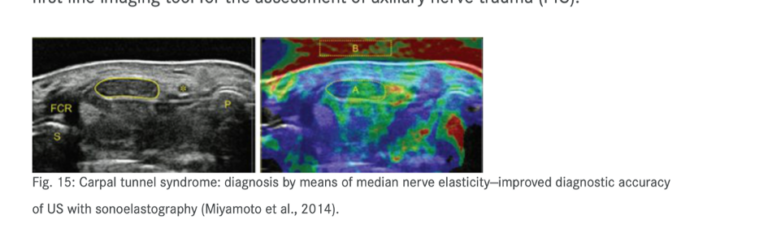
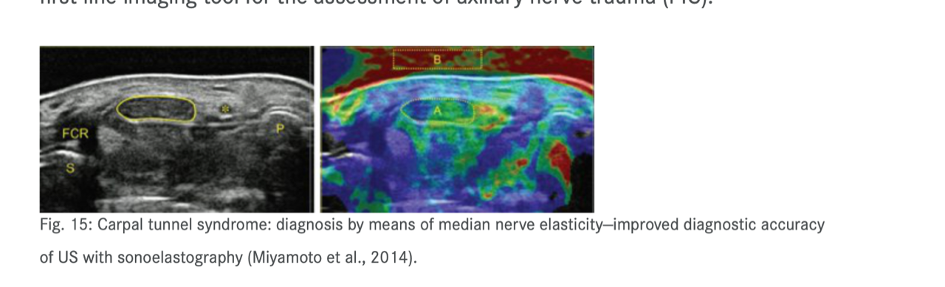
- Sonography of carpal tunnel: definition of cut-off values and correlaztion with Sonoelastography (Fig. 12)
- Sonoelastography of epicondylitis, plantar fasciitis and Achilles tendon: accuracy in comparison with histology
- Sonographically guided (SG) injections in CTS: sonoelastographic appearance
- SG peripheral nerve injection: sonomorphology
- SG nerve entrapment syndromes in comparison with surgical outcome
- SG injection in sacroiliac joints of children: to prove feasibility
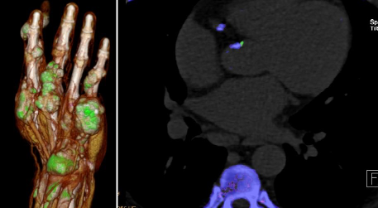
- Dual-energy CT (DECT) in gout: comparison with US- findings, Cardio-DECT in gout and subgroup patients (Fig.13)
- X-ray in comparison with DECT in gout patients
- X-ray in comparison with US in erosion assessment
- MRI in comparison with US in tendon overuse assessment
- MRI whole-spine imaging in inflammatory disease: therapeutic follow-up assessment
- MRI sacroiliitis: therapeutic follow-up assessment
- MR tractography (DTI, ADI) in median nerves of healthy volunteers and CTS patients: comparison with sonography.
Non-Invasive Cardiac/Cardiovascular CT Imaging
Gudrun Feuchtner
a) Coronary heart disease:
atherosclerosis, high-risk plaque marker, risk estimation, algorithms, non-invasive FFR
b) Structural heart disease CT
for planning TAVR, TMVR and catheter ablation, including 3D printing, advanced 3D visualisation, congenital heart disease (Fig. 12).
CT: 10 Multicentre trials

c) Atherosclerotic Burden and its Relevance to Different Diseases and Treatment Strategies.
Bernhard Glodny, Johannes Petersen
Cardiovascular and cerebrovascular sequelae of atherosclerotic disease are among the leading causes of morbidity and mortality in humans. Atherosclerosis can be detected using different modalities of diagnostic imaging. Moreover, treatments are planned by means of clinical imaging, and cardiovascular risk profiles can be compiled individually. CT can be used to quantify the “atherosclerotic burden” of all vascular territories in an objective and reproducible manner.
Relationships between oral health and health in general have been suspected for many years and could also be proven by imaging studies, with evidence of an association between inflammatory changes in the periodontium and increased arteriosclerosis load, thus supporting the concept of arteriosclerosis as an inflammatory disease.
Ultrasound
Hannes Gruber, Alexander Loizides
- Peripheral nerve sonography
- SG interventions in the peripheral nervous system
- SG carpal tunnel release
- Sonographic evaluation of soft tissue masses (incl. MSK contrast-enhanced sonography (CEUS))
- Sonography of the musculoskeletal system
- Sonographic assessment of functional musculoskeletal disorders
- SG pain therapy
- Angiologic assessment and SG interventions in the vascular system
The surgical ultrasound section is a leader in the development of ultrasound techniques for the evaluation of peripheral nerves, ultrasound-guided nerve root infiltration and pain therapy. One of the most recent publications illustrates our work.
The axillary nerve (AN) is frequently injured during shoulder trauma and imaging is required to define the site and extent of nerve injury. However, the AN has a rather complex course through several soft tissue compartments of the shoulder and axilla. Detection and sonographic assessment therefore require thorough knowledge of the local topography.
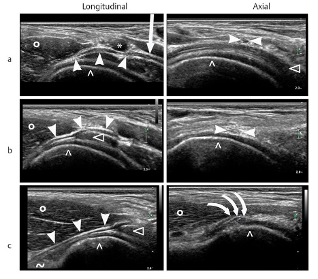
Our investigation aims to define reliable, anatomical landmarks for AN sonography in volunteers and later to validate the proposed sonographic examination protocol in patients. With strict adherence to the proposed examination algorithm, sonography of the AN was feasible in all volunteers and patients. The findings correlated nicely with the gold standard of “surgical exploration” in respect of the severity and topography of neural impairment.
Based on our study results, we propose our algorithm for AN sonography as the first-line imaging tool for the assessment of axillary nerve trauma (PIC).
Interventional Oncology/ Stereotaxy and Robotics
Reto Bale
- Image-guided tumour ablation
- Stereotaxis
- Robotics
- Targeting
- Interventional oncology
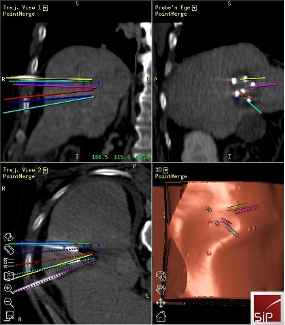
Stereotactic ablation of liver tumours:
Radiofrequency ablation (RFA) allows local curative tumour treatment by inducing coagulation necrosis with a high-frequency alternating current. The major limiting factor of conventional US- and CT- guided percutaneous single probe ablation is the tumour size. Navigation systems allow for 3D-planning of multiple overlapping ablation zones on the CT datasets and precise transformation into the real patient. We developed the worldwide first aiming device for frameless stereotactic punctures and performed the first in man stereotactic radiofrequency ablation (SRFA) of a liver tumor in 2001.
Meanwhile > 1200 patients with > 4500 liver tumors, most of them being inoperable, have successfully been treated at our department. Meanwhile our team has also trained the SMZ Ost in Vienna and the Ordensspital Barmherzige Brüder in Linz. In March 2023 the first stereotactic thermal ablation outside Europe was performed by Prof. Odisio at the MD Anderson in Houston, Texas, USA under supervision of Reto Bale.
Fig. 15: SRFA of a liver tumor with verification of precise needle placement by image fusion (screenshot of 3d navigation system)
Two PhD students from the “Imaged Guided Diagnostics and Therapy – Academic Research Triangle” (IGDT- ART) – funded by the FWF” program are supervised by Matthias Harders from the LFU and Reto Bale:
Adela Moravova: (Semi-)Automatic trajectory planning for multi-probe stereotactic thermal ablation of liver tumors
Stefano Fogarollo: Fast, non-rigid image fusion using deep learning for treatment evaluation after thermal ablation
Genderimaging
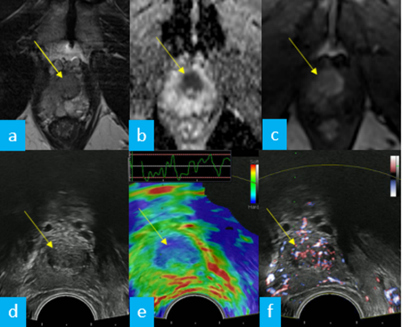
Imaging and Targeted Biopsy of the Genitourinary (GU) Tract
Friedrich Aigner
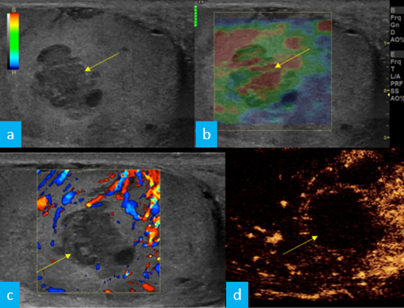
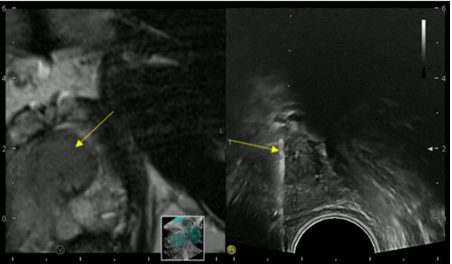
- Multiparametric ultrasound of the scrotum
- Multiparametric ultrasound of the prostate
- Multiparametric MRI of the prostate
- Fusion imaging of the GU-tract
- Fusion targeted biopsy of the prostate
The simultaneous application of structural and functional imaging techniques is described as multiparametric (MP) (Fig. 16). Studies have shown that the MP approach results in greater diagnostic accuracy (Fig. 17).
The use of fusion imaging in uroradiology improves ultrasound lesion-detection rates, shows more reliable size controls at different time points, is an alternative to in-bore biopsies (Fig. 18) and can be used for focal therapy.
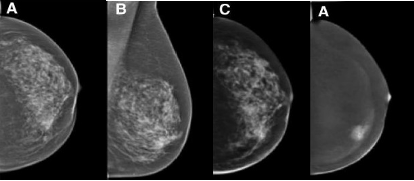
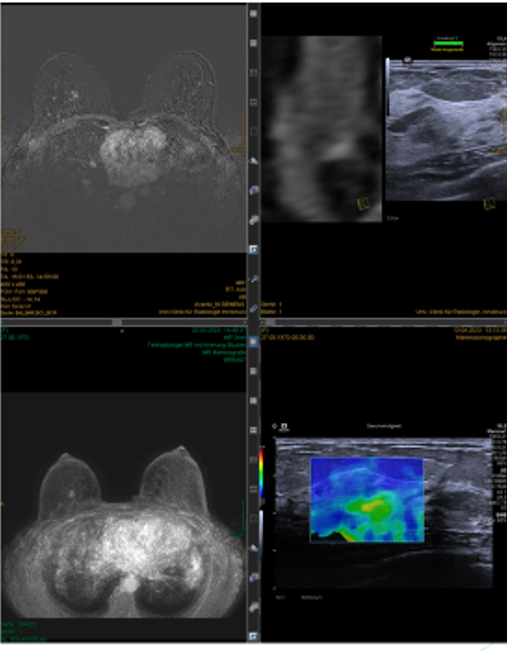
Imaging and Targeted Biopsy of Breast Cancer
Birgit Amort, Leonhard Gruber, Silke Haushammer, Martin Daniaux
The research team focusing on the diagnosis of breast cancer has a vast wealth of experience with all imaging modalities currently used for breast evaluation, including invasive methods such as fine-needle aspirations and/or percutaneous biopsies using stereotaxis or ultrasound guidance. Our unit serves as the largest screening and assessment centre of the national breast-screening programme in Tyrol. Approximately 10.000 mammograms and breast ultrasound studies are performed each year.
The last years have seen the impact of several new research items on daily clinical breast diagnostics routine: Dual-energy (DE) contrast-enhanced mammography is one of the latest developments in breast care. Imaging with contrast agents in breast cancer has been described in MRI and CT. However, high costs, limited availability and high radiation doses have led to the development of contrast-enhanced spectral mammography (CESM), which offers comparable breast cancer detection rates to MRI, yet at a lower false-positive rate, underlining its utility for preoperative local staging. Furthermore, CESM can be used in patients with MRI contraindications.
Increasingly, fusion sonography has been successfully introduced into daily clinical routine and is now employed in cases with sonography-occult findings in MRI and has been repeatedly demonstrated to avoid high-cost and stressful MRI biopsies. Our team has developed special experience to perform such fusion studies even using prone-position breast MRI studies by a more localized landmark-based approach.
RVS ( Real time virtual sonographie) with MRI and CT
Data Management RVS Bioposies
RVS Biopsy vs. MRI Biopsy similar malignacy rate with 20- 29% (Benchmark: 20-50%)
RVS Biopsy: faster, more economical, more comfortable for the patient
Advantages RVS I
RVS enables to find most lesions
Short examination time (~ 10 min.)
Supine position same as standard examination position in ultrasound
Synchronization of two modalities in real time
FOV in supine Pos. < in prone Pos.
Biopsy chest wall and axilla near possible
Advantages RVS II
Biopsy under real time conditions
Selection for MR-biopsies
Significant increase of the detection rate of IELs
Tumor expansion (especially non mass lesions after chemotherapy) more exactly then in B-mode
Real time Ultraschall in Fusionsmodus- IndikationenSecond look-US in incidental enhancing breast lesions (IELs)
Management von km enhancenden Herdläsionen/ non mass Läsionen
Ultraschall gezielte Stanzbiopsie nach RVS
Pictures
Selected Publications
CT Imaging
- Luger AK, Sonnweber T, Gruber L, Schwabl C, Cima K, Tymoszuk P, Gerstner AK, Pizzini A, Sahanic S, Boehm A, Coen M, Strolz CJ, Wöll E, Weiss G, Kirchmair R, Feuchtner GM, Prosch H, Tancevski I, Löffler-Ragg J, Widmann G. Chest CT of Lung Injury 1 Year after COVID-19 Pneumonia: The CovILD Study. 2022 Aug;304(2):462-470.
- Santer M, Kloppenburg M, Gottfried TM, Runge A, Schmutzhard J, Vorbach SM, Mangesius J, Riedl D, Mangesius S, Widmann G, Riechelmann H, Dejaco D, Freysinger W. Current Applications of Artificial Intelligence to Classify Cervical Lymph Nodes in Patients with Head and Neck Squamous Cell Carcinoma-A Systematic Review. Cancers (Basel). 2022 Nov 2;14(21):5397.
- Widmann G, Beyer A, Jaschke W, Luger A, Zoller H, Tilg H, Schneeberger S, Wolf D, Gizewski ER, Eder R, Torbica P, Verius M. Identification and characterization of patients being exposed to computed-tomography associated radiation-doses above 100 mSv in a real-life setting. Eur J Radiol Open. 2022 Dec 21;10:100470. doi: 10.1016/j.ejro.2022.100470. eCollection 2023.
- Widmann G, Schönthaler H, Tartarotti A, Degenhart G, Hörmann R, Feuchtner G, Jacobs R, Pauwels R. As low as diagnostically acceptable dose imaging in maxillofacial trauma: a reference quality approach. Dentomaxillofac Radiol. 2023 Feb;52(3):20220387.
- Widmann G, Dangl M, Lutz E, Fleckenstein B, Offermanns V, Gassner EM, Puelacher W, Salbrechter L. Can ultra-low-dose computed tomography reliably diagnose and classify maxillofacial fractures in the clinical routine? Imaging Sci Dent. 2023 Mar;53(1):69-75.
Experimental Radiology
- Gollmann-Tepeköylü C, Nägele F, Graber M, Pölzl L, Lobenwein D, Hirsch J, An A, Irschick R, Röhrs B, Kremser C, Hackl H, Huber R, Venezia S, Hercher D, Fritsch H, Bonaros N, Stefanova N, Tancevski I, Meyer D, Grimm M, Holfeld J.: Shock waves promote spinal cord repair via TLR3. JCI Insight. 2020; 5(15): e134552.
- García-Martínez, D., Bastir, M., Villa, C. Daniel García-Martínez, Markus Bastir, Chiara Villa, Francisco García-Río, Isabel Torres-Sánchez, Wolfgang Recheis, Alon Barash, Roman Hossein Khonsari, Paul O’Higgins, Marc R. Meyer & Yann Heuzé.: Late subadult ontogeny and adult aging of the human thorax reveals divergent growth trajectories between sexes. Sci Rep 2020, Jul 1;10(1):10737.
- Verius M, Frank F, Gizewski E, Broessner G.: Magnetic Resonance Spectroscopy Thermometry at 3 Tesla: Importance of Calibration Measurements. Ther Hypothermia Temp Manag. 2019;9(2):146-155.
- Empagliflozin protects mice against diet-induced obesity, insulin resistance and hepatic steatosis. Radlinger B, Ress C, Folie S, Salzmann K, Lechuga A, Weiss B, Salvenmoser W, Graber M, Hirsch J, Holfeld J, Kremser C, Moser P, Staudacher G, Jelenik T, Roden M, Tilg H, Kaser S. Diabetologia. 2022 Dec 16. doi: 10.1007/s00125-022-05851-x. Epub ahead of print. PMID: 36525084.
- Morphological and Tissue Characterization with 3D Reconstruction of a 350-Year-Old Austrian Ardea purpurea Glacier Mummy. Unterberger, S.H.; Berger, C.; Schirmer, M.; Pallua, A.K.; Zelger, B.; Schäfer, G.; Kremser, C.; Degenhart, G.; Spiegl, H.; Erler, S.; et al. Biology 2023, 12, 114. https://doi.org/10.3390/biology12010114
Abdominal MR-Imaging
- Henninger B, Alustiza J, Garbowski M, Gandon Y.: Practical guide to quantification of hepatic iron with MRI. Eur Radiol. 2020 Jan;30(1):383-393. doi: 10.1007/s00330-019-06380-9.
- Henninger B, Plaikner M, Zoller H, Viveiros A, Kannengiesser S, Jaschke W, Kremser C.: Performance of different Dixon-based methods for MR liver iron assessment in comparison to a biopsy-validated R2* relaxometry method. Eur Radiol. 2020 Sep 23. doi: 10.1007/s00330-020-07291-w. Online ahead of print.
- Plaikner M, Kremser C, Zoller H, Steurer M, Glodny B, Jaschke W, Henninger B.: Does gadoxetate disodium affect MRE measurements in the delayed hepatobiliary phase? Eur Radiol. 2019 Feb;29(2):829-837.
- 5-T MR relaxometry in quantifying splenic and pancreatic iron: retrospective comparison of a commercial 3D-Dixon sequence and an established 2D multi-gradient echo sequence. Plaikner M, Lanser L, Kremser C, Weiss G, Henninger B. Eur Radiol. 2023 Feb 17. doi: 10.1007/s00330-023-09451-0. Online ahead of print. PMID: 36800012
- Tissue iron distribution in patients with anemia of inflammation: results of a pilot study. Lanser L, Plaikner M, Schroll A, Burkert FR, Seiwald S, Fauser J, Petzer V, Bellmann-Weiler R, Fritsche G, Tancevski I, Duftner C, Pircher A, Seeber A, Zoller H, Kremser C, Henninger B, Weiss G. Am J Hematol. 2023 Jun;98(6):890-899. doi: 10.1002/ajh.26909. Epub 2023 Mar 15. PMID: 36880875.
Cardiovascular MR-Imaging
- Pamminger M, Klug G, Kranewitter C, Reindl M, Reinstadler SJ, Henninger B, Tiller C, Holzknecht M, Kremser C, Bauer A, Jaschke W, Metzler B, Mayr A.: Non-contrast MRI protocol for TAVI guidance: quiescent-interval single-shot angiography in comparison with contrast-enhanced CT. Eur Radiol. 2020 Sept; 30(9): 4847-4856
- A novel approach to determine aortic valve area with phase-contrast cardiovascular magnetic resonance. Troger F, Lechner I, Reindl M, Tiller C, Holzknecht M, Pamminger M, Kremser C, Schwaiger J, Reinstadler SJ, Bauer A, Metzler B, Mayr A, Klug G. J Cardiovasc Magn Reson. 2022 Jan 6;24(1):7. doi: 10.1186/s12968-021-00838-w. PMID: 34986847; PMCID: PMC8734220.
- Prognostic value of pulmonary transit time by cardiac magnetic resonance imaging in ST-elevation myocardial infarction. Pamminger M, Reindl M, Kranewitter C, Troger F, Tiller C, Holzknecht M, Lechner I, Poskaite P, Klug G, Kremser C, Reinstadler SJ, Metzler B, Mayr A. Eur Radiol. 2022 Aug 18. doi: 10.1007/s00330-022-09050-5. Epub ahead of print. PMID: 35980426.
- Cardiac magnetic resonance imaging versus computed tomography to guide transcatheter aortic valve replacement: study protocol for a randomized trial (TAVR-CMR). Klug G, Reinstadler S, Troger F, Holzknecht M, Reindl M, Tiller C, Lechner I, Fink P, Pamminger M, Kremser C, Ulmer H, Bauer A, Metzler B, Mayr A. Trials. 2022 Sep 2;23(1):726. doi: 10.1186/s13063-022-06638-6
- Slice positioning in phase-contrast MRI impacts aortic stenosis assessment. Troger F, Tiller C, Reindl M, Lechner I, Holzknecht M, Pamminger M, Poskaite P, Kremser C, Ulmer H, Gizewski ER, Bauer A, Reinstadler S, Metzler B, Klug G, Mayr A. Eur J Radiol 2023; 161, 110722. https://doi.org/10.1016/j.ejrad.2023.110722
Imaging and Targeted Biopsy of the Genitourinary (GU) Tract
- Do we need repeated CT imaging in uncomplicated blunt renal injuries? Experiences of a high-volume urological trauma centre.
Lindner AK, Luger AK, Fritz J, Stäblein J, Radmayr C, Aigner F, Rehder P, Tulchiner G, Horninger W, Pichler R.
World J Emerg Surg. 2022 Jul 7;17(1):38. doi: 10.1186/s13017-022-00445-9. - Enlarged cardiophrenic lymph nodes predict disease involvement of the upper abdomen and the outcome of primary surgical debulking in advanced ovarian cancer. Luger AK, Steinkohl F, Aigner F, Jaschke W, Marth C, Zeimet AG, Reimer D. Acta Obstet Gynecol Scand. 2020 Feb 29. doi: 10.1111/aogs.13835. [Epub ahead of print] PMID: 32112653
- Multiparametric ultrasound in torsion of the testicular appendages: a reliable diagnostic tool? Laimer G, Müller R, Radmayr C, Lindner AK, Lebovici A, Aigner F. Med Ultrason. 2021 Sep 11. doi: 10.11152/mu-3206. Online ahead of print. PMID: 34508618
Imaging and Targeted Biopsy of Breast Cancer
- Preoperative staging by multimodal imaging in newly diagnosed breast cancer: Diagnostic performance of contrast-enhanced spectral mammography compared to conventional mammography, ultrasound, and MRI. Daniaux M, Gruber L, De Zordo T, Geiger-Gritsch S, Amort B, Santner W, Egle D, Baltzer PAT.Eur J Radiol. 2023 Jun;163:110838. doi: 10.1016/j.ejrad.2023.110838. Epub 2023 Apr 15.PMID: 37080064
- Interval breast cancer: Analysis of occurrence, subtypes and implications for breast cancer screening in a model region. Daniaux M, Gruber L, Santner W, Czech T, Knapp R.Eur J Radiol. 2021 Oct;143:109905. doi: 10.1016/j.ejrad.2021.109905. Epub 2021 Aug 10.PMID: 34403883
- Geiger-Gritsch S, Daniaux M, Buchberger W, Knapp R, Oberaigner W.: Performance of 4 years of population-based mammography screening for breast cancer combined with ultrasound in Tyrol / Austria. Wien Klin Wochenschr. 2018 Feb;130(3-4):92-99.
- van Dam PA, Tomatis M, Marotti L, Heil J, Mansel RE, Rosselli Del Turco M, van Dam PJ, Casella D, Bassani LG, Danei M, Denk A, Egle D, Emons G, Friedrichs K, Harbeck N, Kiechle M, Kimmig R, Koehler U, Kuemmel S, Maass N, Mayr C, Prové A, Rageth C, Regolo L, Lorenz-Salehi F, Sarlos D, Singer C, Sohn C, Staelens G, Tinterri C, Audisio R, Ponti A; eusomaDB Working Group.: Time trends (2006-2015) of quality indicators in EUSOMA-certified breast centres. Eur J Cancer. 2017 Nov;85:15-22.
- Oberguggenberger A, Martini C, Huber N, Fallowfield L, Hubalek M, Daniaux M, Sperner-Unterweger B, Holzner B, Sztankay M, Gamper E, Meraner V.: Self-reported sexual health: Breast cancer survivors compared to women from the general population – an observational study. BMC Cancer. 2017 Aug 30;17(1):599.
Musculoskeletal Imaging
- Klauser AS, Halpern EJ, Strobl S, Gruber J, Feuchtner G, Bellmann-Weiler R, Weiss G, Stofferin H, Jaschke W.: Dual-Energy Computed Tomography Detection of Cardiovascular Monosodium Urate Deposits in Patients With Gout. JAMA Cardiol. 2019 Oct 1;4(10):1019-1028.
- Strobl S, Kremser C, Taljanovic M, Gruber J, Stofferin H, Bellmann-Weiler R, Klauser AS.: Impact of Dual-Energy CT Postprocessing Protocol for the Detection of Gouty Arthritis and Quantification of Tophi in Patients Presenting With Podagra: Comparison With Ultrasound. AJR Am J Roentgenol. 2019 Dec;213(6):1315-1323.
- Sconfienza LM, Adriaensen M, Albano D, Allen G, Aparisi Gómez MP, Bazzocchi A, Beggs I, Bignotti B, Chianca V, Corazza A, Dalili D, De Dea M, Del Cura JL, Di Pietto F, Drakonaki E, Facal de Castro F, Filippiadis D, Gielen J, Gitto S, Gupta H, Klauser AS, Lalam R, Martin S, Martinoli C, Mauri G, McCarthy C, McNally E, Melaki K, Messina C, Mirón Mombiela R, Neubauer B, Olchowy C, Orlandi D, Plagou A, Prada Gonzalez R, Rutkauskas S, Snoj Z, Tagliafico AS, Talaska A, Vasilevska-Nikodinovska V, Vucetic J, Wilson D, Zaottini F, Zappia M, Obradov M.: Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part I, shoulder. Eur Radiol. 2020 Feb;30(2):903-913.
- Evaluation of Classic and Quantitative Imaging Features in the Differentiation of Benign and Atypical Lipomatous Soft Tissue Tumors Using a Standardized Multiparametric MRI Protocol: A Prospective Single-Centre Study in 45 Patients. Gruber, L., Kremser, C., Zelger, B., Schwabegger, A., Josip, E., Dammerer, D., Thaler, M., Henninger, B. Curr. 2023, 30, 3315–3328. https://doi.org/10.3390/curroncol30030252
Non-invasive Cardiac/Cardiovascular CT-Imaging
- Feuchtner GM, Barbieri F, Luger A, Skalla E, Kountchev J, Widmann G, Plank F.: Myocardial injury in COVID-19: The role of coronary computed tomography angiography (CTA). J Cardiovasc Comput Tomogr. 2020 Jul 17:S1934-5925(20)30391-9. Epub ahead of print.
- Feuchtner G, Langer C, Barbieri F, Beyer C, Dichtl W, Friedrich G, Schgoer W, Widmann G, Plank F.: The effect of omega-3 fatty acids on coronary atherosclerosis quantified by coronary computed tomography angiography. Clin Nutr. 2020 Jul 22:S0261-5614(20)30381-2.
- van Rosendael AR, Narula J, Lin FY, van den Hoogen IJ, Gianni U, Al Hussein Alawamlh O, Dunham PC, Peña JM, Lee SE, Andreini D, Cademartiri F, Chinnaiyan K, Chow BJW, Conte E, Cury RC, Feuchtner G, Hadamitzky M, Kim YJ, Leipsic J, Maffei E, Marques H, de Araújo Gonçalves P, Plank F, Pontone G, Raff GL, Villines TC, Weirich HG, Al’Aref SJ, Baskaran L, Cho I, Danad I, Han D, Heo R, Lee JH, Rivzi A, Stuijfzand WJ, Gransar H, Lu Y, Sung JM, Park HB, Samady H, Stone PH, Virmani R, Budoff MJ, Berman DS, Chang HJ, Bax JJ, Min JK, Shaw LJ.: Association of High-Density Calcified 1K Plaque With Risk of Acute Coronary Syndrome. JAMA Cardiol. 2020 Mar 1;5(3):282-290
Ultrasound
- Gruber H, Jaschke W, Loizides A.: Ultrasound Guidance for Pleural-Catheter Placement. N Engl J Med. 2018 Jul 26;379(4):401.
- Differentiation of Critical Illness Myopathy and Critical Illness Neuropathy Using Nerve Ultrasonography. Gruber L, Loizides A, Gruber H, Skalla E, Haushammer S, Horlings C, Beer R, Helbok R, Löscher WN.J Clin Neurophysiol. 2022 Jan 25. doi: 10.1097/WNP.0000000000000922. Online ahead of print.PMID: 35089907
Interventional Oncology/ Stereotaxy and Robotics
- Schullian P, Laimer G, Johnston E, Putzer D, Eberle G, Widmann G, Scharll Y, Bale R.: Reliability of Stereotactic Radiofrequency Ablation (SRFA) for Malignant Liver Tumors: Novice versus Experienced Operators. Biology (Basel). 2023 Jan 22;12(2):175. doi: 10.3390/biology12020175.
- Scharll Y, Letrari S, Laimer G, Schullian P, Bale R.: Puncture accuracy of an optical tracked robotic aiming device-a phantom study. Eur Radiol. 2022 Oct;32(10):6769-6776. doi: 10.1007/s00330-022-08915-z.
- Schullian P, Laimer G, Johnston E, Putzer D, Eberle G, Scharll Y, Widmann G, Kolbitsch C, Bale R.: Technical efficacy and local recurrence after stereotactic radiofrequency ablation of 2653 liver tumors: a 15-year single-center experience with evaluation of prognostic factors. Int J Hyperthermia. 2022;39(1):421-430. doi: 10.1080/02656736.2022.2044522
- Laimer G, Schullian P, Bale R.: Stereotactic Thermal Ablation of Liver Tumors: 3D Planning, Multiple Needle Approach, and Intraprocedural Image Fusion Are the Key to Success-A Narrative Review. Biology (Basel). 2021 Jul 10;10(7):644. doi: 10.3390/biology10070644.
- Laimer G, Jaschke N, Schullian P, Putzer D, Eberle G, Solbiati M, Solbiati L, Goldberg SN, Bale R.: Volumetric assessment of the periablational safety margin after thermal ablation of colorectal liver metastases. Eur Radiol. 2021 Sep;31(9):6489-6499. doi: 10.1007/s00330-020-07579-x. Erratum in: Eur Radiol. 2021 Jun 17;: PMID: 33447860
Selection of Funding
Selection of Competitive Acquired Funding
- 2021: FWF grand: “Image Guided Diagnosis and Therapy” (DOC 110-B): Coordinator of PhD projects Prof. Elke R. Gizewski & Prof. Clemens Decristoforo
- MITIGATE #602306: Closed-loop Molecular Environment for Minimally Invasive Treatment of Patients with metastatic Gastrointestinal Stromal Tumours; EU FP7; -Prof. Dr. Werner Jaschke
- EUCLID: European Study on Clinical Diagnostic Reference Levels for X-ray Medical Imaging; Europ. Commission: Contracnr. EC Tender ENER/2017/NUCL/SI2.759174; Univ.-Prof. Dr. Elke R. Gizewski, em.o.Univ.-Prof. Dr. Werner Jaschke, Dr. Michael Verius
- VASCage-C: Imaging Biomarkers For Vascular Diseases And Vascular Aging; COMET K1 Zentren 4.Call: 1. FP Partner (FFG), Projektnummer: 6401616; Univ.-Prof. Dr. Elke R. Gizewski, Assoz.-Prof. PD Dr. Bernhard Glodny, PD Dr. Wolfgang Recheis, Assoz.-Prof. PD Dr. Astrid E. Grams, Dr. Ruth Steiger, Dr. Sergiy Pereverzyev Jr.
- Subproject Vascage: Post-Stroke Osteopathie; Degenhart Gerald MSc BSc
- KM-induziertes Nierenversagen bei chron. Niereninsuffizienz im Schweinemodell: „CIN- Pig“; MFF Tirol #265; Dr. Anna-Katharina Luger, Assoz.-Prof. PD Dr. Bernhard Glodny
- Basic evaluation of a contrast-free pre-TAVI imaging option: first comparison of a new native MRI protocol with standard-ized contrast-enhanced CT; GHKF Gesellschaft zur Förderung der Herz-Kreislaufforschung in Tirol; -Prof. PD Dr. Agnes Mayr
- Long term evolution of infarct scar after reperfused ST-segment elevation myocardial infarction: a 10 year Follow-Up Cardiac Magnetic Resonance Study; ÖKG Österreichische Kardiologische Gesellschaft; Assoz.-Prof. PD Dr. Agnes Mayr
- DISCHARGE Trial : Diagnostic Imaging Strategies: Invasive versus coronary computed tomography angiography for stable chest pain patients with intermediate risk of coronary artery disease: a multicentric randomized pragmatic trial.; 7th Framework Programme (Grant No. 603266) of the European Union.; Ao. Univ.-Prof. Dr. Gudrun Feuchtner
- MedCorpInn – Retrospective Intersectional Corpuslinguistic Analysis of Radiology and Medical Reports of Medical University of Innsbruck; Austrian Academy of Sciences, go!digital 2.0; Mag. Dr. Claudia Posch (University of Innsbruck, Institute for Linguistics), Karoline Irschara, MA (University of Innsbruck, Institute for Linguistics), med. univ. Leonhard Gruber, PhD (Universitätsklinik für Radiologie, Medizinische Universität Innsbruck), Dr.in med. univ. Stephanie Mangesius, PhD (Universitätsklinik für Neuroradiologie, Medizinische Universität Innsbruck)
Collaborations
Siemens Healthcare Erlangen
Interventional Systems, Kitzbühel
Medtronic, Boulder, USA
Leopold Franzens Universität Innsbruck
Institut für Geologie : Fachbereich Sedimentologie: Univ.-Prof. Dr. Michael Strasser
Institut für Mineralogie und Petrographie: Ao.Univ.-Prof. Dr. Peter Tropper
Institut für Archäologien : Fachbereich Ur-und Frühgeschichte sowie Mittelalter- und Neuzeitarchäologie: Univ.-Prof. Dr. Harald Stadler; Fachbereich Klassische und Provinzialrömische Archäologie: Mag. Dr. Ulrike Töchterle, Mag. Dr. Martin Auer
Institut für Sprachwissenschaft: Ass.Prof. Mag. Dr. Claudia Posch, Karoline Irschara, MA
Applied Mathematics: Univ.-Prof. Dr. Markus Haltmeier
Eidgenössische Technische Hochschule Zürich: Institut für Biomechanik: Univ. Prof. Dr. Ralph Müller
Universitätsklinikum Ulm: Institut für Unfallchirurgische Forschung und Biomechanik: Univ. Prof. Dr. Anita Ignatius
Johannes Keppler Universität: Institut für Physiologie & Pathophysiologie: Univ. Prof. Dr. Jakob Völkl
Landesmuseum Ferdinandeum: Mag.phil. Wolfgang Sölder
Kelten Museum Hallein: Margarethe Kirchmayr, MA
National Taiwan University: Jyh-Jaan Huang PHD (momentan Forschungsaufenthalt an der LFU Innsbruck)
ASTC Axel Schnaller Technologie Consult
Managementcenter Innsbruck: Mechatronik- Medizintechnik: Dr. techn. Franz- Josef Falkner
Cardiac gout project with DECT: multicenter collaboration with Rheumatology Department at Vancouver General Hospital (VGH) and Massachusetts General Hospital (MGH)
MSK ultrasound collaborations with Thomas Jefferson University, PA and Department of Medical Imaging, The University of Arizona Health Network
MSK Imaging collaborations with Diagnostic and Interventional Radiology, Istituto Ortopedico Galeazzi, Italy
Novartis Institutes for Biomedical research, Biomarker Development- Clinical Imaging
Basel, Switzerland: Tendon stiffness as a biomarker to quantify tendon healing after Achilles tendon rupture (2016). Projektnummer (Powertrials 1302): Director Didier Laurent, PhD