Anichstraße 35
6020 Innsbruck
Fax: +43 512 504 27096
Email: neuroradiologie@i-med.ac.at
Website: http://radiologie.tirol-kliniken.at/
Research Branch (ÖSTAT Classification)
301111, 301401, 302010, 302043, 302044, 302070, 302071, 302079
Keywords
artificial intelligence, dose management, DTI, dual-energy-CT, fMRI, High-field MRI, interventional neuroradiology, MR-spectroscopy, multimodal imaging, and quantitative MR-imaging
Research Focus
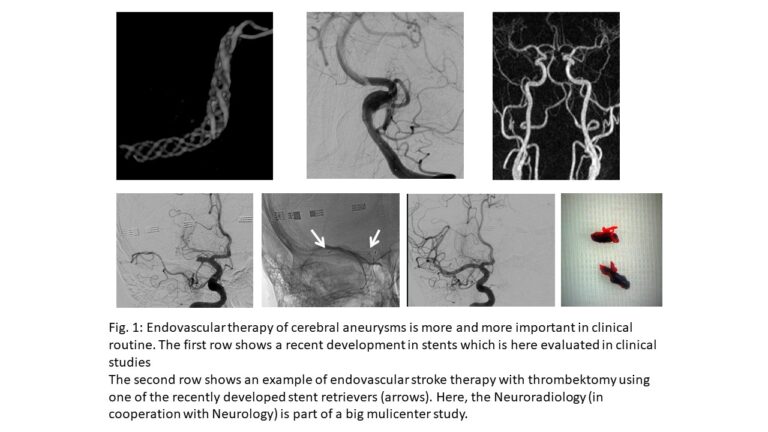
To a large extent, neuro-radiological research is connected with and driven by its clinical partners (Neuro-Focus at MUI) as well as other departments (clinical and theoretical) at MUI, MCI, UMIT and LFU. Projects generated within Neuroradiology focus mostly on technical developments (dose reduction / dual-energy CT, MRI sequence and post-processing developments, fMRI/VBM, multi-nuclear MRI), some in cooperation with the Department of Radiology. Furthermore, Neuroradiology conducts clinical studies, e.g. into neurovascular disease (Fig. 1. Within recent years, the research focus extended to multimodal, quantitative MRI and artificial intelligence applications on neuro-radiological imaging.
General Facts
Structure to the Research Unit, Aims and Clinical Routine
Together with the Department of Radiology, neuroradiology is involved in radiographer and physician training programmes as well as research and routine clinical activities. The two departments have a long-standing PhD programme (Image-Guided Diagnosis & Therapy) and a clinical PhD programme (Clinical Imaging Science). In 2021, a FWF grand for the “Image Guided Diagnosis and Therapy” programme (DOC 110-B) was achieved. Within this programme, together with the Departments of Nuclear Medicine, ENT, Radiation Therapy and Oncology and Medical Physics, the research expertise was increased by mathematics, computer science and engineering including partners from LFU (Applied Mathematics and Computer Science) and from UMIT (Biomedical Engineering).
Neuroradiology has a large clinical workload, which includes all diagnostic and interventional neurology cases of paediatric and adult patients, resulting in many clinically related research projects in imaging and intervention (including interventional EU studies). The senior physicians and one assoc. Professor teach the younger colleagues and PhD students in all aspects of research education, supported by the scientists of the Core Facility for Neuroimaging Research (CF-NIR) including MR physics, advanced mathematics and artificial intelligence. This leads to new insights in scanning, image analysis and follow-up prognoses.
The experimental research relates mainly to the CF-NIR, but also to many national and international cooperative partners with long-standing expertise in fMRI, ultra-high field MRI (7T in cooperation with the imaging unit of DKFZ Heidelberg), multimodal, multi-nuclear and quantitative imaging. Imaging of cerebral processing related to cognitive and emotional stimuli with respect to possible gender differences relates partly to psychiatric research and partly to projects in critical emotional situations in cardiology.
Research
This section lists only those research projects that are headed mainly by Neuroradiology.
Training in Interventional Radiology – What Can We Learn from Aviation?
Dr. Ouaret, Assoz.-Prof. Grams
The introduction of standard procedures and checklists, as well as simulation training, as soon as they became available in the aviation industry in the 1950s and 60s, significantly increased aviation safety. The paradigm shift in medicine is a very slow process.
This project’s target is to explore whether an aviation style approach to teaching in Interventional Neuroradiology could revolutionise teaching by establishing guidelines to certain procedures and a cockpit simulation training environment.
Dual-Energy CT in Stroke Patients
Assoz.-Prof. Grams, Dr. Mangesius, Dr. Eisenschink in cooperation with Prof. Kiechl, Prof. Knoflach and Prof. Haltmeier (LFU)
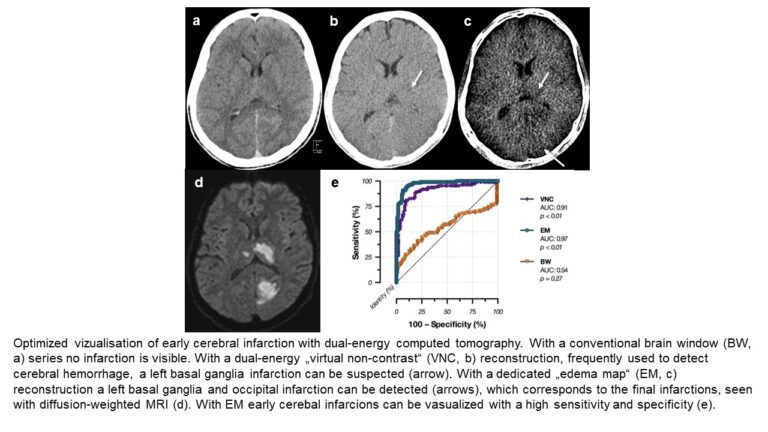
The detection of acute cerebral infarction is crucial in order to decide on further treatment. By comparison with conventional CT, early infarctions can be better identified with dual-energy CT (Fig. 2).
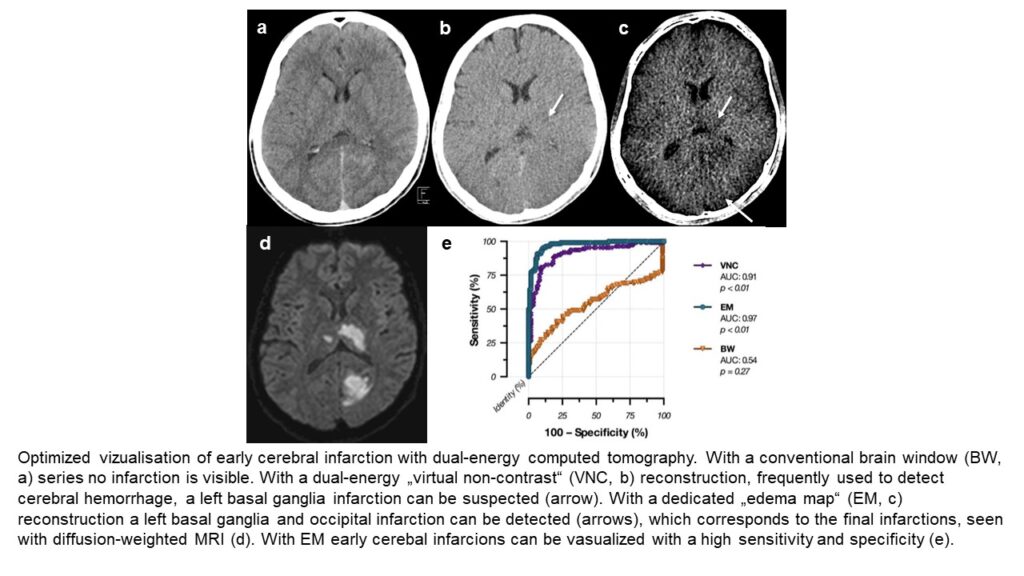
A recent research project aims to predict infarction development prior to its visualisation by using radiomics features in dual-energy CT datasets.
Aneurysm Wall Enhancement in Cerebral Aneurysms
Assoc.-Prof. Dr. Grams, Dr. Ladenhauf and Prof. Gizewski in cooperation with PD Dr. Helbok
The purpose of this project involving patients with treated or untreated cerebral aneurysms is to investigate aneurysm wall enhancement. The presence, frequency and severity of enhancements under different circumstances and correlation with aneurysm reperfusion will be investigated.
MRI and MRS Parameters in the Cerebral Development of Preterm Infants
Prof. Gizewski and Dr. Pereverzyev in cooperation with Prof. Kiechl-Kohlendorfer and Prof. Buchheim (LFU)
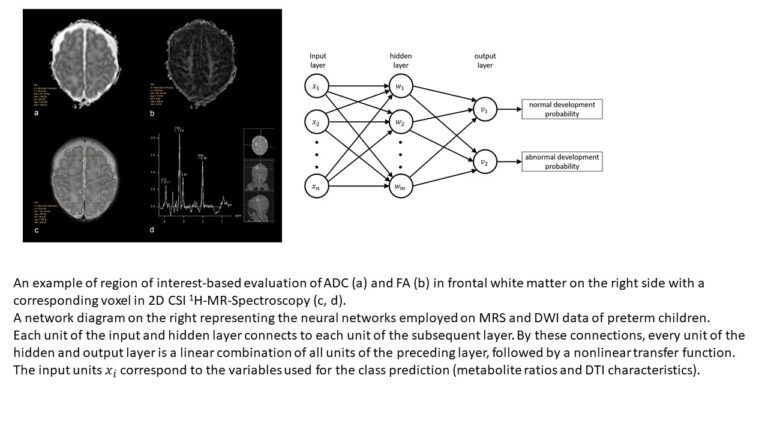
In this prospective study of multimodal MRI in very preterm neonates (< 32 gestational weeks), we employed feed-forward neural networks (fNNs), a segment of artificial intelligence. We showed that fNNs can be a useful predictive tool for cognitive and motor outcome prediction in very preterm neonates by using cerebral 1H-MrS and DTI biomarkers (Fig. 3).
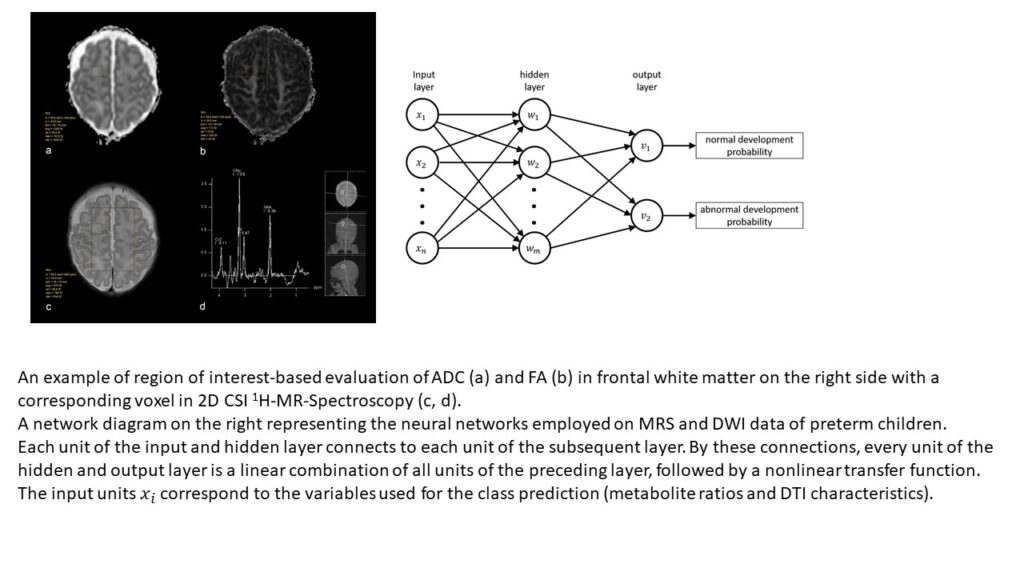
Moreover, by combining these sophisticated methods, the predictive value of MRI can be significantly increased. Further applications are now being tested in a larger cohort.
31P MRS in Cerebral Gliomas and Metastases
Assoc.-Prof. Grams, Dr. Galijasevic, Dr. Mangesius, Prof. Gizewski, and Dr. Steiger in cooperation with Prof. Thomé, Dr. Kerschbaumer, Doz. Freyschlag, Doz. Nowosielski and Prof. Nevinny-Stickel
By using MR spectroscopy of phosphorus compounds (31P MRS), it is possible to detect metabolites of energy metabolism and of membrane turnover. 31P MRS is used in patients with cerebral gliomas and metastases, to investigate tumour heterogeneity and the effects of therapy not only on the tumorous area, but also on the healthy brain hemisphere. The resulting data will be correlated with results obtained from established methods, such as 1H MRS, MR perfusion, DWI and clinical, histological and PET parameters.
31P MRS in Stroke Patients
Assoc.-Prof. Grams, Dr. Sommer and Dr. Steiger in cooperation with Prof. Kiechl and Prof. Knoflach
31P MRS is used in patients with acute, subacute and chronic ischemic stroke to gain further insights into the energy metabolism and reorganisation mechanisms of infarcted brain and surrounding areas during the acute stage and to monitor subacute and chronic changes.
MR Spectroscopy in well-characterised individuals with and without post COVID condition prior to and following a Yoga breathing or control intervention- an Explorative randomised controlled trial.
Prof. Dr. Elke R. Gizewski, Prof. Dr. Barbara Sperner-Unterweger, Prof. Dr. Judith Löffler-Ragg, Prof. Dr. Nicolas Singewald, Mag. Michaela Waibel, PD Dr. Johanna Gostner, Dr. Alessandra Fanciulli, Dr. Alexander Karabtsiakis, Prof. Dr. Katharina Hüfner et al.
From a clinical perspective, we find that many patients with Post COVID condition suffer from severe and debilitating shortness of breath, while routine pulmonary investigations fail to find the cause of the problems experienced. If dyspnoea is associated with palpitations, dizziness or anxiety, patients are commonly diagnosed with “dysfunctional breathing”. From a psychosomatic perspective, the symptom of dysfunctional breathing can be classified as a “functional symptom” under the umbrella term of somatic symptom disorder. Therefore, Yoga interventions with special emphasis on breath-guided relaxation are a promising approach. We aim to investigate the psycho-somatic and somato-psychic pathophysiology on a morphological, psychological, functional and biological basis underlying the symptom of dysfunctional breathing. Furthermore, we plan to investigate the mechanism of Yoga intervention on the mental and somatic symptom burden of participants with Post COVID condition. Subsequently, we aim to compare the impact of Yoga on other groups – healthy individuals, patients with chronic obstructive lung disease (COPD), as well as those with somatic symptom disorder. As a control intervention to Yoga guided breathing exercises, a social contact group will be used.
Contribution of Myelin to the Diamagnetic Susceptibility of Normal and Multiple Sclerosis (MS) Brain
DI Dr. Birkl (Erwin-Schrödinger Fellow) in cooperation with Prof. Haybeck
Although a wide spectrum of MRI techniques is available to assess the density and integrity of myelin, the detailed contribution of its different constituents in relation to magnetic susceptibility is still only partially understood. A novel technique called Quantitative Susceptibility Mapping (QSM) allows assessment of the magnetic susceptibility of biological tissue using MRI. The strongest contributors to magnetic susceptibility of the human brain are iron and myelin. The main aim of this project is to uncover the influence of myelin (Myelin Water Imaging – MWI) and its different components on the magnetic susceptibility of healthy and MS brain tissue.
Imaging Markers for Tissue Damage and Disease Progression in MS
DI Dr. Birkl and Prof. Rauscher (University of British Columbia, Canada)
There is still a lack of advanced MRI tools for early MS diagnosis, monitoring of disease progression and quantification of tissue repair from MS drugs currently under development. Our broad aim is to quantify tissue damage in MS by means of QSM and MRI signal decay (R2*). The aim of this project is to establish white matter fibre orientation-dependent R2* as an imaging marker for disease progression in MS. For this approach, we calculate R2* as a function of white matter fibre orientation. By matching a computational model of iron and myelin to experimental data, we are able to determine the average total content of white matter iron and myelin.
Towards Quantitative Neuroimaging Biomarkers for Friedreich’s ataxia at 7 Tesla
Prof. Gizewski and Dr. Mangesius in cooperation with the German Cancer Research Centre, Heidelberg (Dr. Straub and Prof. Ladd) and PD Dr. Bösch (Neurology Innsbruck)
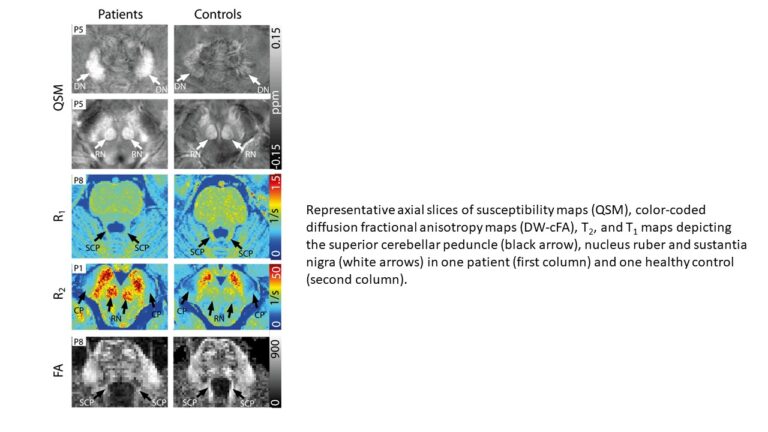
Modern imaging processes and new imaging techniques with ultra-high field 7T MRI are being investigated. FRDA leads to degenerative cerebral processes. So far, no effective treatment has been found. It is therefore important to aid the development of mediation with imaging biomarkers that reflect disease status and progress. MRI data for QSM, R1, R2* and DWI have been acquired at 7T and have facilitated the identification of statistically significant differences between FRDA patients and controls in five out of twelve brain investigated structures (Fig. 4)
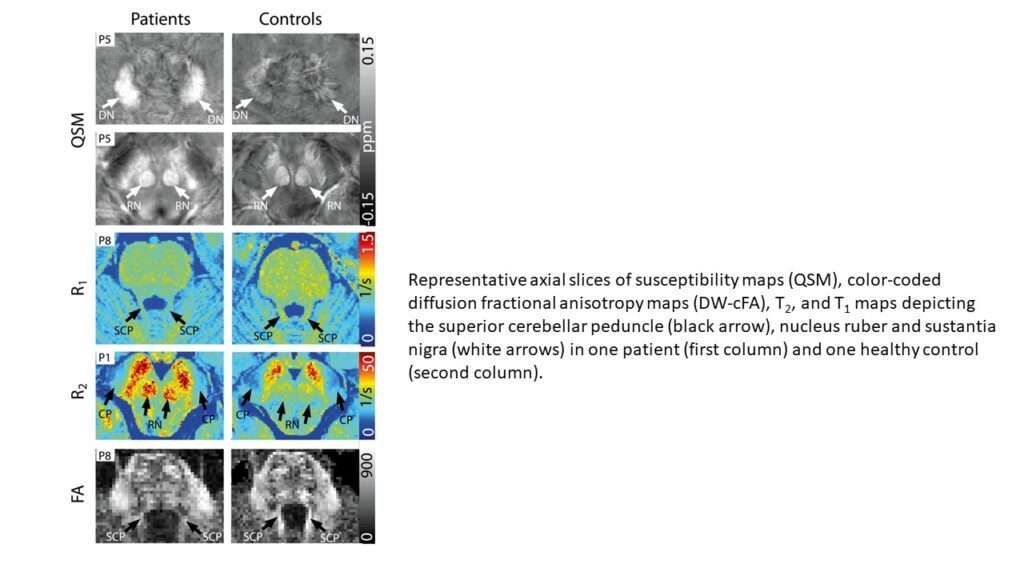
, which also correlated positively with disease characteristics. Future studies will include the application of these markers in routinely applied 3T field strengths and the investigation of asymptomatic mutation carriers.
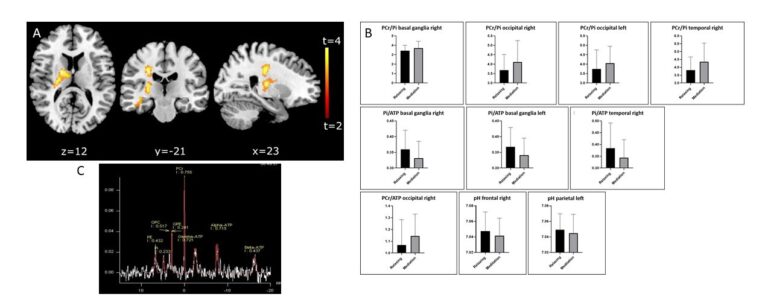
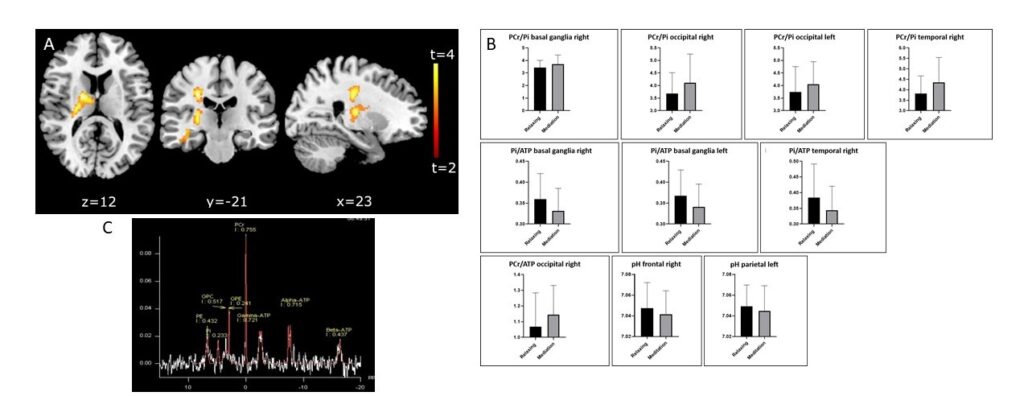
Effect of Short-Term Meditation Training on Brain Metabolism, Function and Volume
Prof. Gizewski, Dr. Steiger, Dr. Lenhart, Dr. Mangesius, Dr. Siedentopf, Dr. Pereverzyev and Dr. Galijasevic in cooperation with Prof. Singewald (LFU)
Meditation is increasingly attracting interest among neuroimaging researchers on the basis of its relevance as a cognitive enhancement technique. This longitudinal study applies a distinct and standardised meditative technique with a group of volunteers in a short-term training programme, in order to analyse brain metabolic, functional and structural changes. Initial results indicate that meditation may have considerable effects on the brain energy state with different local energy management in specific brain regions, and may alter cerebral grey and white matter mainly in the insula, caudate nucleus, frontal cortices, parietotemporal regions, right medial prefrontal cortex, basal ganglia and parahippocampal gyrus (Fig. 5).
Applied mathematics
Dr. Pereverzyev Jr. in cooperation with the clinical researchers at the CF-NIR
Apart from the research activities concerning various fundamental questions in applied mathematics, this topic includes sections of the modern mathematical applications in radiology. Herein, the prediction of an object’s state using object’s characteristics is considered. For this prediction, techniques of machine learning are employed. In the next section, methods for accurate and low inter-user variable segmentations of anatomical structures in MR images are developed.
Comparison of software applications
Prof. Gizewski, Dr. Mangesius, Dr. Lenhart, Dr. Steiger
With the advance of precision medicine, numerous open source and commercial software applications have evolved to allow automated and thus potentially fast and unbiased measurement of brain volumes. To date, none of these approaches has emerged as a gold standard in clinical routine or research. Hence, the measurement of atrophy in routine clinical practice remains an unmet need. Additionally, while these applications have been repeatedly shown to be highly consistent within them, consistency has remained less clear when being compared to each other. Yet, this point is most relevant for consistency across both clinical care providers and across research groups in the search for imaging markers. The present study quantifies the agreement across different software applications for different neurological diseases with degenerative aspects.
MR planimetric measurements for diagnosis and outcome prediction of Multiple Sclerosis
Prof. Gizewski, Dr. Mangesius and Dr. Pereverzyev Jr. in cooperation with Prof. Deisenhammer (Neurology Innsbruck)
The advent of MRI provided a powerful tool for monitoring the dynamics of pathological changes in multiple sclerosis, but conventional approaches offer only limited, often subjective information that is directly relevant to clinical progression. Continued developments of imaging methods and their use for diagnosis, monitoring pathology and understanding disease progression are of interest. The main objective of this study is therefore to investigate whether the simple and easily applicable MR planimetry can predict the technically more complex volumetric measurements at baseline and at follow-up examinations.
Deep Learning for automated segmentation of head and neck vasculature and outcome prediction of ischemic stroke with Dual-Energy CT
Prof. Gizewski, Dr. Mangesius and Dr. Pereverzyev Jr. in cooperation with Prof. Neumann (LFU)
In this work, we intent to program an automated method for cerebral vascular segmentation that does not require initialising seed points or other manual intervention and can be applied to any imaging modality, which will then be tested on both MRA and CTA data. This method should account for the differences in intensity in homogeneities and tissue/bone contrast in MR and CT data and includes extensive validation using 3D Convolutional Neural Networks. We furthermore hypothesise that radiomic features extracted from DECT images can serve as an even better prognostic factor for the prediction of future infarct size, haemorrhagic transformations and to further determine clinical outcome by applying deep learning and artificial intelligence methods employing radiomics features for predicting probabilities.
Two PhD students of our IGDT-ART programme are also involved in this study and will finish their thesis within this project.
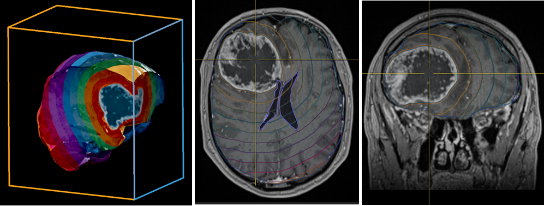
Advanced imaging techniques for monitoring treatment response in patients with primary brain tumours and cerebral metastases after radiotherapy
Prof. Gizewski, Dr. Mangesius and Dr. Birkl in cooperation with Prof. Ganswindt and Dr. Mangesius (Radiooncology Innsbruck), PD Freyschlag, Dr. Kerschbaumer, Dr. Pinggera and Prof. Thomé (Neurosurgery Innsbruck), PD Uprimny (Nuclear Medicine Innsbruck) and Prof. Haybaeck (Neuropathology Innsbruck)
Evaluating treatment response after radiation of brain metastases and primary brain tumours can be challenging despite state-of-the-art imaging techniques. Differentiation of tumour progression from treatment-related effects (radiation necrosis and pseudo-progression) is crucial to select the correct treatment as early as possible. Currently, a definitive diagnosis can often only be achieved by invasive brain biopsy. This study’s aim is 1. to implement an image analysis pipeline locally for monitoring treatment response in patients after cerebral radiotherapy using quantitative imaging techniques, thus enabling a more accurate and earlier non-invasive differentiation, and 2. to investigate tumour effects on normal appearing white matter in order to anticipate treatment outcome. This approach might enable early and correct treatment decisions, thus offer the best individual medical care and potentially improving patient prognosis and quality of life. (Fig. 6)
![Fig. 6b: Comparison of the 3 imaging modalities deployed in this study. Left: [18F] FET PET. Middle: T1 MPRAGE contrast enhanced MRI. Right: Contrast Clearance Analysis.](https://researchreport.i-med.ac.at/wp-content/uploads/2023/09/Folie6_Teil2.png)
Pictures
Selected Publications
- Marto JP; Strambo D; Ntaios G; Nguyen TN; Herzig R; Czlonkowska A ; Demeestere J; Mansour OY ; Salerno A; Wegener S; Baumgartner P; Cereda CW; Bianco G; Beyeler M; Arnold M; Carrera E; Machi P; Altersberger V; Bonati L; Gensicke H; Bolognese M; Peters N; Wetzel S; Magriço M; Ramos JN; Sargento-Freitas J; Machado R; Maia C; Machado E; Nunes AP; Ferreira P; Pinho e Melo T; Carvalho Dias M; Paula A; Correia MA; Castro P; Azevedo E; Albuquerque L; Alves JN; Ferreira-Pinto J; Meira T; Pereira L; Rodrigues M; Pinho Araujo A; Rodrigues M; Rocha M; Pereira-Fonseca A; Ribeiro L; Varela R; Malheiro S; Cappellari M; Zivelonghi C; Sajeva G; Zini A; Gentile M; Forlivesi S; Migliaccio L; Sessa M; La Gioia S; Pezzini A; Sangalli D; Zedde M; Pascarella R; Ferrarese C; Beretta S; Diamanti S; Schwarz G; Frisullo G; Marcheselli S; Seners P; Sabben C; Escalard S; Piotin M; Maïer B; Charbonnier G; Vuillier F; Legris L; Cuisenier P; Vodret FR; Marnat G; Liegey J-S; Sibon I; Flottmann F; Broocks G; Gloyer N-O; Bohmann FO; Schaefer JH; Nolte C; Audebert HJ; Siebert E; Sykora M; Lang W; Ferrari J; Mayer-Suess L; Knoflach M; Gizewski ER; et al (2023). Safety and Outcome of Revascularization Treatment in Patients With Acute Ischemic Stroke and COVID-19: The Global COVID-19 Stroke Registry. Neurology, Feb 14;100(7):e739-e750
- Mangesius S; Haider L; Lenhart L; Steiger R; Carrasco FP; Scherfler C; Gizewski ER (2022). Qualitative and quantitative comparison of hippocampal volumetric software applications: Do all roads lead to Rome? Biomedicines, 12; 10(2): 432.
- Galijašević M, Steiger R, Radović I, Birkl-Toeglhofer AM, Birkl C, Deeg L, Mangesius S, Rietzler A, Regodić M, Stockhammer G, Freyschlag CF, Kerschbaumer J, Haybaeck J, Grams AE, Gizewski ER (2021). Phosphorus Magentic Resonance Spectroscopy and Molecular Markers in IDH1 Wild Type Glioblastoma. Cancers (Basel). 2021 Jul 16;13(14):3569
- Gruber N; Galijasevic M; Regodic M; Grams AE; Siendentopf C; Steiger R; Hammerl M; Haltmeier M; Gizewski ER; Janjic T (2022). A deep learning pipeline for the automated segmentation of posterior limb of internal capsule in preterm neonates. Artificial Intelligence in Medicine, 2022 Oct;132:102384
- Grams AE, Mangesius S, Steiger R, Radovic I, Rietzler A, Walchhofer LM, Galijašević M, Mangesius J, Nowosielski M, Freyschlag CF, Kerschbaumer J, Gizewski ER. Changes in Brain Energy and Membrane Metabolism in Glioblastoma following Chemoradiation. Curr Oncol. 2021 Dec 1;28(6):5041-5053. doi: 10.3390/curroncol28060424.
Selection of Funding
- FWF grand for the “Image Guided Diagnosis and Therapy” programme: DOC 110-B: IGDT – integrating multimodal strategies for clinical research: Coodinator: Gizewski, Co-Coordinator Decristoforo
- FFG COMET programme: Gizewski: PI Subproject “Imaging biomarkers for vascular disease and vascular ageing”, K1 Centre Tirol: VASCage-C (Centre for the Promotion of Vascular Health in the Ageing Community)
- Mangesius and Schiefeneder anniversary fund: “Automatisierte MR-Planimetrie-Messungen zur Diagnose und Prognose von Multipler Sklerose” (Automated MR planimetry measurements for multiple sclerosis diagnosis and prognosis)
Collaborations
- Austria: NEUROIMAGE WING (BMWFW grand: pooled MRI data collection and analysis Med. Universities Innsbruck, Graz, Vienna (Neurology and Neuroradiology, 7T MRI)
- Innsbruck: Prof. Baumgarten, Biomedical Informatics and Mechatronics (UMIT)
- Markus Haltmeier, Applied Mathematics (LFU), Prof. Matthias Harders, Interactive Graphics and Simulation (LFU)
- Anna Buchheim and Team, Clinical Psychology (LFU)
- Nicolas Singewald, Neuropharmacology (LFU)
- Germany: University Hospital Essen (Medical Psychology & Behavioural Immunobiology, Radiology), Erwin L. Hahn Institute Essen (Prof. Harald Quick)
- DKFZ Heidelberg / MR Imaging (Prof. Mark Ladd)
- Dresden Technical University (Prof. Jennifer Linn, Neuroradiology), Hamburg University (Prof. Jens Fiehler, Neuroradiology)
- Switzerland: Hirslanden Clinic Zürich, Prof. Isabel Wanke, Prof. Daniel Rüfenacht, Neuroradiology
- Canada: University of British Columbia (Biomedical Imaging)
- Siemens Healthineers (Erlangen, Germany), Kinepict Health Ltd. (Budapest, Hungary