Co Director: Univ.-Prof. Dr.med.univ. Gerald Brandacher
Anichstraße 35
6020 Innsbruck
Email: Stefan.Schneeberger@i-med.ac.at
Website: https://www.chirurgie-innsbruck.at/
Research year
Research Branch (ÖSTAT Classification)
106023, 301114, 301904, 302003, 302082, 302083
Keywords
cancer, cryopreservation, immunomodulation, ischemia-reperfusion injury, machine perfusion, microbiome, organ preservation, quality assurance, translational oncology, and transplantation
Research Focus
Clinical and Molecular Oncology
Translational research focuses on the tumorigenic effects of altered intracellular signalling pathways and the role of fungal dysbiosis in the development of pancreatic ductal adenocarcinomas.
Organ Preservation, Transplantation, and Inflammation
Experimental and clinical machine perfusion, along with cryopreservation of organs, biochemical, functional imaging and bioenergetic assessment provide the foundation for a comprehensive evaluation and treatment of organs during preservation.
Quality Assurance in Surgery
Our comprehensive, quality-controlled registry is the foundation for advancing the magnitude and quality of clinical studies and translational research.
General Facts
The Department of Visceral, Transplant and Thoracic Surgery (VTT) maintains a high-volume adult and paediatric transplant programme that is internationally established and renowned for its innovation and excellence. It covers all solid organs as well as vascularised composite allografts. The second focus is on oncology. We are the specialists in solutions for all types of tumours. Whatever the surgery, whether abdominal, endocrine, breast or thoracic, we have the experience to help. Our high-volume cancer care is internationally renowned. It is interlinked with corresponding research programmes and forms part of an auditable quality assurance programme, which represents a separate scientific focus.
Daniel Swarovski Transplantation Research Laboratory
The Daniel Swarovski Research Laboratory (DSL) was established to add an equally ambitious research focus to the comprehensive solid organ transplantation programme initiated by Prof. Raimund Margreiter. The main research focus is on ice-free subzero organ preservation using nature-inspired cryoprotectants. Our goal is to alleviate one of the most daunting challenges and limitations in the field of transplantation, namely, the extremely limited time for organ preservation.
organLifeTM Laboratory
The organLifeTM laboratory is a multidisciplinary research core unit for machine perfusion of all organs. It is also an assessment platform that allows in-depth analysis of organ viability, function, and regeneration. Our primary objective is to establish long-term organ preservation.
Research
Research Focus: Oncology
Clinical Oncology
The clinical oncology group is involved in the planning and implementing of national and international clinical studies. These include several phase-II and III studies (MORIP-AIMS study, RAW-study, DREAM study, E-MIPS registry, SLASA and SOLE study). The group is developing prognostic scores (ASPEN study, ASSO pNEN study group, ADENO-IPMN-2 study), which are validated by international centres. Recent efforts have led to the formation of the Austrian Association for Hepato-Pancreato-Biliary Surgery (AAHPBS) and the biennial European consensus meetings on liver surgery.
Molecular Oncology
Tissue Microarrays and Organoids
Tissue microarrays and organoids from a large cohort of pancreatic, lung and colorectal cancer samples provide a solid foundation for gaining mechanistic insights into the molecular aspects of tumour development and progression.
Microbiota and Fungal Dysbiosis
We are currently investigating the commensal gut fungus Malassezia globosa in collaboration with the Institute of Hygiene and Medical Microbiology. Our research focuses on its interaction with the host immune response and its role in pancreatic tumorigenesis.
Leveraging Normothermic Liver Machine Perfusion (NLMP) as a Platform for Oncologic Assessment and Drug Development
We retrieve the cirrhotic livers of patients undergoing liver transplantation for HCC during surgery. We cool and flush them with Custodiol® solution. Subsequently, after reconstructing the venous outflow, we initiate NLMP. We have thereby, for the first time, demonstrated the feasibility of perfusing a cirrhotic liver carrying an HCC using a commercially available NLMP device. This technology is the foundation for a key ex situ tumour model that will serve as a platform for further drug development and refinement.
Research Focus: Organ Preservation, Transplantation and Inflammation
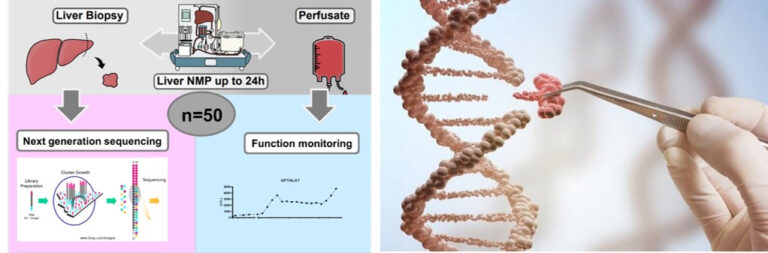
Molecular Mechanisms and Biomarkers During Liver NMP
Since 2018, our group has performed over 350 liver NMPs. We identified transcriptomic signatures during NMP by using NGS. An inflammatory response and ischemia/reperfusion injury were evident early after NMP, but tissue repair and anti-inflammatory pathways were induced with prolonged NMP. We have identified PDL1 as a new biomarker that reliably predicts graft quality. Furthermore, the immune cell repertoire and its dynamic changes were evaluated during liver NMP.
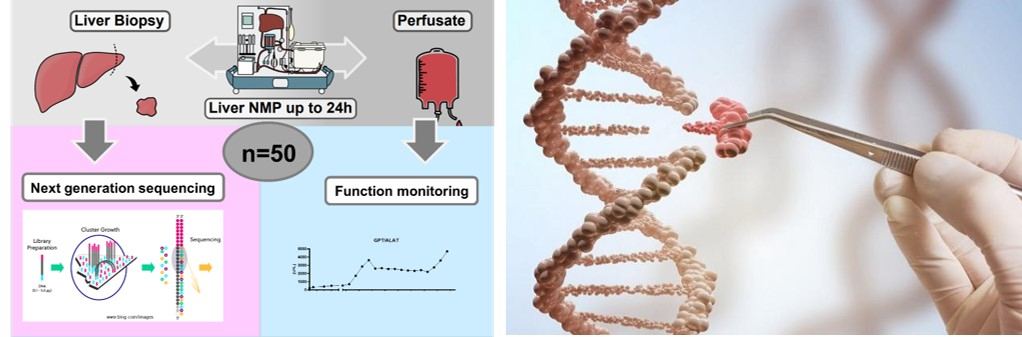
These findings establish the ground for active immune modulation during liver NMP.
Long-term Liver NMP
The organLifeTM project was initiated with the main goal of establishing long-term organ perfusion. In 2024, our protocol was granted a patent, paving the way for one-week liver NMP. Long-term NMP offers the potential for modification, regeneration, and repair of marginal grafts.
AAV Gene Delivery in Liver NMP
Liver-directed adeno-associated virus (AAV) vectors are a promising candidate for the treatment of liver genetic diseases, but highly-specific AAV vectors are lacking. We are developing optimised AAV vectors to treat familial hypercholesterolemia as part of a project supported by VASCage/FFG (hLDLR gene transfer, together with Dept.of Virology and Lysomb).
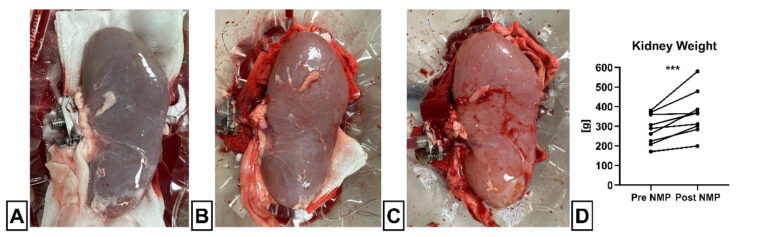
Developing a Novel Kidney NMP Device
We use a kidney perfusion device to assess the impact of 24h NMP on kidneys. Our findings show the potential of NMP for prolonged organ preservation and as a quality assessment tool. Since 2021, organLife has been working with the US company DEKA to develop a cutting-edge instrument for comprehensive assessment of quality and function of perfused kidneys.
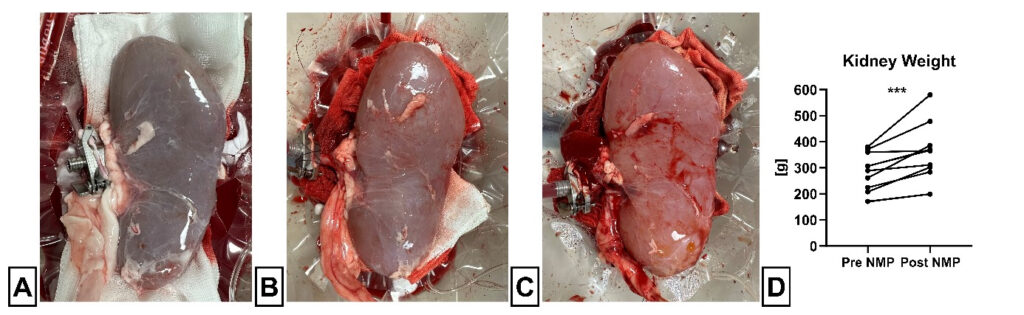
weight (organLifeTM Laboratory)
Ice-free Subzero Organ Preservation
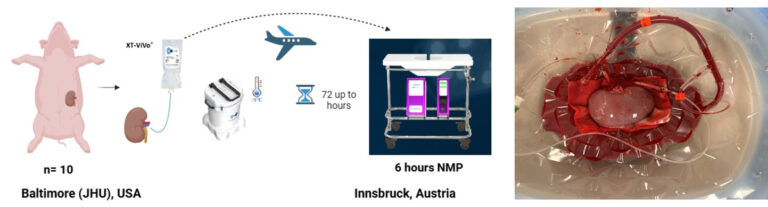
In collaboration with the team at X-Therma Inc., we are working on innovative technologies that focus on developing transformational new tissue and organ preservation techniques. These techniques include the use of nature-inspired, next-generation cryoprotective agents (chemically engineered anti-freeze proteins/peptoid oligomers). These agents allow for ice-free preservation of organs (kidney, liver, heart) at subzero temperatures. In 2024, a world first, a pig kidney was preserved at -5C and successfully transported by our team across the Atlantic Ocean, demonstrating the potential for this novel technology to greatly extend organ storage and preservation, and make long-distance organ transportation a clinical reality. Specifically, a kidney was recovered from a pig at the Johns Hopkins University School of Medicine in Baltimore, Maryland, USA and transported on a commercial aircraft to the MUI. The kidney was preserved for 48 hours at subzero temperatures, and was assessed in the organLife laboratory using NMP and demonstrated viability and functionality.
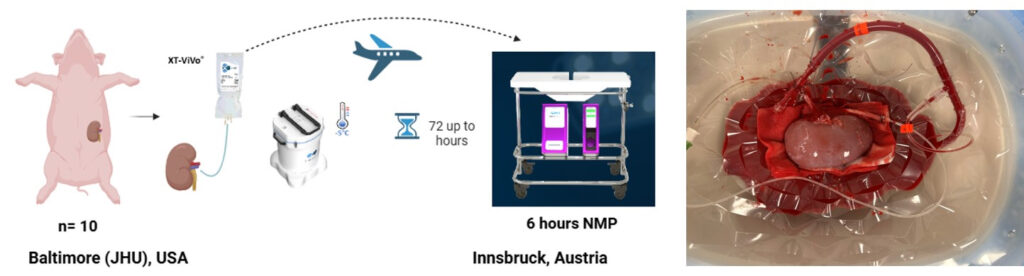
reperfusion after 48h of preservation at -5C on the Kidney Assist devise (right).
Pig kidneys are retrieved at The Johns Hopkins University in Baltimore and cooled and stored for up to 72h in a special designed cooling device prototype, called TimeSeal©. During the storage, the organ is transported to the OrganLife Lab in Innsbruck via plane. Here, we subject the organ to 6 hour NMP, using gradual rewarming as well as a pressure protocol during the first hour of perfusion. (Daniel Swarovski Transplantation Laboratory (DSL), organLifeTM Laboratory)
Research Focus: Thoracic Surgery
The thoracic surgery group is focused on cutting-edge surgical interventions, translational research and clinical innovations aimed at improving outcomes of thoracic malignancies, lung transplantation and other related conditions. The group is involved in multi-disciplinary collaborations, integrating surgical advancements with oncology, immunology, computer science and biomedical engineering. Using minimally invasive and robotic-assisted thoracic surgery, the role of predictive modelling in lung cancer surgery, leveraging large datasets and AI-driven analytics to determine patient-specific surgical strategies that optimise survival rates and minimise complications are major areas of investigation. Research in lung transplantation focuses on ex-vivo lung perfusion (EVLP) to assess and optimise donor lung function prior to transplantation.
Research Focus: Quality Assurance in Surgery
Our digital, proprietary quality assurance programme is the result of more than 30 years of experience. It provides quality-controlled, audit-ready data in routine clinical practice. The department’s clinical data pool with more than 130,000 patient records is a unique feature and serves as an indispensable tool, for several retrospective studies. It provides reliable data for national and international registries. Current research explores how deep machine learning (AI) can be used to further process the plethora of data.
Pictures
Selected Publications
Research Focus Oncology
Rangelova E, Stoop TF, van Ramshorst TME, Ali M, van Bodegraven EA, Javed AA, Hashimoto D, Steyerberg E, Banerjee A, Jain A, Sauvanet A, Serrablo A, Giani A, Giardino A, Zerbi A, Arshad A, Wijma AG, Coratti A, Zironda A, Socratous A, Rojas A, Halimi A, Ejaz A, Oba A, Patel BY, Björnsson B, Reames BN, Tingstedt B, Goh BKP, Payá-Llorente C, Del Pozo CD, González-Abós C, Medin C, van Eijck CHJ, de Ponthaud C, Takishita C, Schwabl C, Månsson C, Ricci C, Thiels CA, Douchi D, Hughes DL, Kilburn D, Flanking D, Kleive D, Silva DS, Edil BH, Pando E, Moltzer E, Kauffman EF, Warren E, Bozkurt E, Sparrelid E, Thoma E, Verkolf E, Ausania F, Giannone F, Hüttner FJ, Burdio F, Souche FR, Berrevoet F, Daams F, Motoi F, Saliba G, Kazemier G, Roeyen G, Nappo G, Butturini G, Ferrari G, Kito Fusai G, Honda G, Sergeant G, Karteszi H, Takami H, Suto H, Matsumoto I, Mora-Oliver I, Frigerio I, Fabre JM, Chen J, Sham JG, Davide J, Urdzik J, de Martino J, Nielsen K, Okano K, Kamei K, Okada K, Tanaka K, Labori KJ, Goodsell KE, Alberici L, Webber L, Kirkov L, de Franco L, Miyashita M, Maglione M, Gramellini M, Ramera M, Amaral MJ, Ramaekers M, Truty MJ, van Dam MA, Stommel MWJ, Petrikowski M, Imamura M, Hayashi M, D’Hondt M, Brunner M, Hogg ME, Zhang C, Suárez-Muñoz MÁ, Luyer MD, Unno M, Mizuma M, Janot M, Sahakyan MA, Jamieson NB, Busch OR, Bilge O, Belyaev O, Franklin O, Sánchez-Velázquez P, Pessaux P, Holka PS, Ghorbani P, Casadei R, Sartoris R, Schulick RD, Grützmann R, Sutcliffe R, Mata R, Patel RB, Takahashi R, Rodriguez Franco S, Cabús SS, Hirano S, Gaujoux S, Festen S, Kozono S, Maithel SK, Chai SM, Yamaki S, van Laarhoven S, Mieog JSD, Murakami T, Codjia T, Sumiyoshi T, Karsten TM, Nakamura T, Sugawara T, Boggi U, Hartman V, de Meijer VE, Bartholomä W, Kwon W, Koh YX, Cho Y, Takeyama Y, Inoue Y, Nagakawa Y, Kawamoto Y, Ome Y, Soonawalla Z, Uemura K, Wolfgang CL, Jang JY, Padbury R, Satoi S, Messersmith W, Wilmink JW, Abu Hilal M, Besselink MG, Del Chiaro M; European Consortium on Minimally Invasive Pancreatic Surgery (E-MIPS); International Consortium on Advanced Pancreatic Surgery. The impact of neoadjuvant therapy in patients with left-sided resectable pancreatic cancer: an international multicenter study. Ann Oncol. 2025 Jan 13:S0923-7534(25)00004-3. doi: 10.1016/j.annonc.2024.12.015. Epub ahead of print. PMID: 39814200.
Andel PCM, van Goor IWJM, Augustinus S, Berrevoet F, Besselink MG, Bhojwani R, Boggi U, Bouwense SAW, Cirkel GA, van Dam JL, Djanani A, Dorcaratto D, Dreyer S, den Dulk M, Frigerio I, Ghorbani P, Goetz MR, Groot Koerkamp B, Gryspeerdt F, Hidalgo Salinas C, Intven M, Izbicki JR, Jorba Martin R, Kauffmann EF, Klug R, Liem MSL, Luyer MDP, Maglione M, Martin-Perez E, Meerdink M, de Meijer VE, Nieuwenhuijs VB, Nikov A, Nunes V, Pando E, Radenkovic D, Roeyen G, Sanchez-Bueno F, Serrablo A, Sparrelid E, Tepetes K, Thakkar RG, Tzimas GN, Verdonk RC, Ten Winkel M, Zerbi A, Groot VP, Molenaar IQ, Daamen LA, van Santvoort HC; European-African Hepato-Pancreato-Biliary Association. Routine Imaging or Symptomatic Follow-Up After Resection of Pancreatic Adenocarcinoma. JAMA Surg. 2025 Jan 1;160(1):74-84. doi: 10.1001/jamasurg.2024.5024.
Krendl FJ, Cardini B, Zoller H, Schneeberger S, Oberhuber R. Leveraging normothermic liver machine perfusion as a platform for oncologic assessment in cirrhotic livers. J Hepatol. 2025 Jan;82(1):e12-e14. doi: 10.1016/j.jhep.2024.08.027. Epub 2024 Aug 31. PMID: 39836511.
Primavesi F, Maglione M, Cipriani F, Denecke T, Oberkofler CE, Starlinger P, Dasari BVM, Heil J, Sgarbura O, Søreide K, Diaz-Nieto R, Fondevila C, Frampton AE, Geisel D, Henninger B, Hessheimer AJ, Lesurtel M, Mole D, Öllinger R, Olthof P, Reiberger T, Schnitzbauer AA, Schwarz C, Sparrelid E, Stockmann M, Truant S, Aldrighetti L, Braunwarth E, D’Hondt M, DeOliveira ML, Erdmann J, Fuks D, Gruenberger T, Kaczirek K, Malik H, Öfner D, Rahbari NN, Göbel G, Siriwardena AK, Stättner S. E-AHPBA-ESSO-ESSR Innsbruck consensus guidelines for preoperative liver function assessment before hepatectomy. Br J Surg. 2023 Sep 6;110(10):1331-1347. doi: 10.1093/bjs/znad233. PMID: 37572099; PMCID: PMC10480040.
Bellotti R, Paiella S, Primavesi F, Jäger C, Demir IE, Casciani F, Kornprat P, Wagner D, Rösch CS, Butturini G, Giardino A, Goretzky PE, Mogl M, Fahlbusch T, Kaiser J, Strobel O, Nießen A, Luu AM, Salvia R, Maglione M. Treatment characteristics and outcomes of pure Acinar cell carcinoma of the pancreas – A multicentric European study on radically resected patients. HPB (Oxford). 2023 Nov;25(11):1411-1419. doi: 10.1016/j.hpb.2023.07.897. Epub 2023 Jul 27. PMID: 37563033.
Research Focus: Organ Preservation, Transplantation and Inflammation
Hautz T, Hackl H, Gottschling H, Gronauer R, Hofmann J, Salcher S, Zelger B, Oberhuber R, Cardini B, Weissenbacher A, Resch T, Troppmair J, Schneeberger S. Transcriptomic signatures during normothermic liver machine perfusion correspond with graft quality and predict the early graft outcome. EBioMedicine. 2024 Sep 18;108:105330. doi: 10.1016/j.ebiom.2024.105330.
Hofmann J, Meszaros AT, Butler A, Hann A, Hartog H, Kneifel F, Iype S, Crick K, Cardini B, Fiore B, Attia M, Pollok JM, Pascher A, Vogel T, Perera T, Watson CJE, Schneeberger S. Predictive value of early postoperative lactate (<6 h) during normothermic machine perfusion and outcome after liver transplantation: results from a multicentre study. Br J Surg. 2024 Jun 12;111(6):znae084. doi: 10.1093/bjs/znae084.
Hofmann J, Meszaros AT, Buch ML, Nardin F, Hackl V, Strolz CJ, Zelger B, Fodor M, Cardini B, Oberhuber R, Resch T, Weissenbacher A, Troppmair J, Schneeberger S, Hautz T. Bioenergetic and Cytokine Profiling May Help to Rescue More DCD Livers for Transplantation.
Int J Mol Sci. 2023 May 31;24(11):9536. doi: 10.3390/ijms24119536.
Hautz T, Salcher S, Fodor M, Sturm G, Ebner S, Mair A, Trebo M, Untergasser G, Sopper S, Cardini B, Martowicz A, Hofmann J, Daum S, Kalb M, Resch T, Krendl F, Weissenbacher A, Otarashvili G, Obrist P, Zelger B, Öfner D, Trajanoski Z, Troppmair J, Oberhuber R, Pircher A, Wolf D, Schneeberger S. Immune cell dynamics deconvoluted by single-cell RNA sequencing in normothermic machine perfusion of the liver. Nat Commun. 2023 Apr 21;14(1):2285. doi: 10.1038/s41467-023-37674-8.
Krendl FJ, Cardini B, Fodor M, Singh J, Ponholzer F, Messner F, Weissenbacher A, Resch T, Maglione M, Margreiter C, Eschertzhuber S, Irsara C, Griesmacher A, Schennach H, Breitkopf R, Schlosser L, Zoller H, Tilg H, Oberhuber R, Schneeberger S. Normothermic Liver Machine Perfusion At a Large European Center -Real World Outcomes Following 238 Applications. Ann Surg. 2025 Jan 20. doi: 10.1097/SLA.0000000000006634. Epub ahead of print. PMID: 39829417.
Rabelink TJ, Hosgood S, Minor T, Selzner M, Weissenbacher A, Leuvenink HG, Schneeberger S. Opportunities and challenges with the implementation of normothermic machine perfusion in kidney transplantation. Nat Commun. 2025 Jul 25;16(1):6883. doi: 10.1038/s41467-025-60410-3.
Esser H, de Jong IEM, Roos FM, Bogensperger C, Brunner SM, Cardini B, Dutkowski P, Eker H, Ferreira-Gonzalez S, Forbes SJ, Friend PJ, Fundora Y, Junger H, Krendl FJ, Martins PN, de Meijer VE, Oberhuber R, Oniscu GC, Patrono D, Porte RJ, Resch T, Sadik H, Schlegel A, De Stefano N, Vidgren M, Watson CJE, Weißenbacher A, Schneeberger S. Consensus classification of biliary complications after liver transplantation: guidelines from the BileducTx meeting. Br J Surg. 2025 Apr 30;112(5):znae321. doi: 10.1093/bjs/znae321.
Krendl FJ, Cardini B, Zoller H, Schneeberger S, Oberhuber R. Leveraging normothermic liver machine perfusion as a platform for oncologic assessment in cirrhotic livers. J Hepatol. 2025 Jan;82(1):e12-e14. doi: 10.1016/j.jhep.2024.08.027. Epub 2024 Aug 31.
Esser H, Kilpatrick AM, Man TY, Aird R, Rodrigo-Torres D, Buch ML, Boulter L, Walmsley S, Oniscu GC, Schneeberger S, Ferreira-Gonzalez S, Forbes SJ. Primary cilia as a targetable node between biliary injury, senescence and regeneration in liver transplantation. J Hepatol. 2024 Dec;81(6):1005-1022. doi: 10.1016/j.jhep.2024.06.002. Epub 2024 Jun 13.
Krendl FJ, Resch T, Eschertzhuber S, Schneeberger S, Oberhuber R. Normothermic liver machine perfusion as a dynamic platform for assessment and treatment of organs from a donor with malaria – expanding the indications. J Hepatol. 2024 Nov;81(5):e236-e237. doi: 10.1016/j.jhep.2024.07.031. Epub 2024 Jul 31.
Krendl FJ, Cardini B, Laimer G, Singh J, Resch T, Oberhuber R, Schneeberger S. Normothermic Liver Machine Perfusion and Successful Transplantation of Split Liver Grafts: From Proof of Concept to Clinical Implementation. Transplantation. 2024 Jun 1;108(6):1410-1416. doi: 10.1097/TP.0000000000004997. Epub 2024 May 23.
Fodor M, Zelger P, Pallua JD, Huck CW, Hofmann J, Otarashvili G, Pühringer M, Zelger B, Hermann M, Resch T, Cardini B, Oberhuber R, Öfner D, Sucher R, Hautz T, Schneeberger S. Prediction of Biliary Complications After Human Liver Transplantation Using Hyperspectral Imaging and Convolutional Neural Networks: A Proof-of-concept Study. Transplantation. 2024 Feb 1;108(2):506-515. doi: 10.1097/TP.0000000000004757. Epub 2024 Jan 19.
Mathis S, Weissenbacher A, Putzer G, Gasteiger L, Cardini B, Hell T, Schlosser L, Oberhuber R, Schneeberger S, Martini J. Interleukin-6 Levels During Normothermic Machine Perfusion Impact Postreperfusion Hemodynamics of Liver Graft Recipients: A Prospective Single-center Observational Study. Transplantation. 2024 May 1;108(5):1166-1171. doi: 10.1097/TP.0000000000004852. Epub 2024 Apr 24.
Krendl FJ, Bellotti R, Sapisochin G, Schaefer B, Tilg H, Scheidl S, Margreiter C, Schneeberger S, Oberhuber R, Maglione M. Transplant oncology – Current indications and strategies to advance the field. JHEP Rep. 2023 Nov 16;6(2):100965. doi: 10.1016/j.jhepr.2023.100965. eCollection 2024 Feb.
Resarch Focus Thoracic Surgery
Ponholzer F, Bogensperger C, Krendl FJ, Krapf C, Dumfarth J, Schneeberger S, Augustin F. Beyond the organ: lung microbiome shapes transplant indications and outcomes. European Journal of Cardio-Thoracic Surgery. 2024 Sep. 17:ezae338. doi: 10.1093/ejcts/ezae338
Salcher S, Sturm G, Horvath L, Untergasser G, Kuempers C, Fotakis G, Panizzolo E, Martowicz A, Trebo M, Pall G, Gamerith G, Sykora M, Augustin F, Schmitz K, Finotello F, Rieder D, Perner S, Sopper S, Wolf D, Pircher A, Trajanoski Z. High-resolution single-cell atlas reveals diversity and plasticity of tissue-resident neutrophils in non-small cell lung cancer. Cancer Cell. 2022 Dec 12;40(12):1503-1520.e8. doi: 10.1016/j.ccell.2022.10.008. Epub 2022 Nov 10. PMID: 36368318; PMCID: PMC9767679.
Abram J, Spraider P, Martini J, Velik-Salchner C, Dejaco H, Augustin F, Putzer G, Hell T, Barnes T, Enk D. Flow-controlled versus pressure-controlled ventilation in thoracic surgery with one-lung ventilation – A randomized controlled trial. J Clin Anesth. 2025 Feb 27;103:111785. doi: 10.1016/j.jclinane.2025.111785. Epub ahead of print. PMID: 40020438.
Ponholzer F, Dumfarth J, Krapf C, Pircher A, Hautz T, Wolf D, Augustin F, Schneeberger S. The impact and relevance of techniques and fluids on lung injury in machine perfusion of lungs. Front. Immunol. 2024 Mar 06;15:1358153. doi: 10.3389/fimmu.2024.1358153
Ponholzer F, Schweiger T, Ghanim B, Maier H, Hutter J, Tomaselli F, Krause A, Müller M, Lindenmann J, Spruk G, Augustin F. Analysis of Pain Management after Anatomic VATS Resection in Austrian Thoracic Surgery Units. J Clin Med. 2023 Dec 22;13(1):80. doi: 10.3390/jcm13010080
Mildner FO, Sykora MM, Hackl H, Amann A, Zelger B, Sprung S, Buch ML, Nocera F, Moser P, Maier H, Augustin F, Manzl C, Kocher F, Pircher A, Lindenmann J, Mykoliuk I, Raftopoulou S, Kargl J, Wolf D, Sopper S, Gamerith G. Soluble PD-L1 shows no association to relapse and overall survival in early stage non-small cell lung cancer (NSCLC). Lung Cancer. 2024 Oct;196:107955. doi: 10.1016/j.lungcan.2024.107955. Epub 2024 Sep 16. PMID: 39306924.
Terbuch A, Konjic S, Schlintl V, Absenger G, Jost PJ, Lindenmann J, Swatek P, John N, John T, Wurm R, Zacharias M, Posch F, Hochmair MJ, Fabikan H, Weinlinger C, Illini O, Horvath L, Gamerith G, Wolf D, Augustin F, Brcic L. Prognostic impact of targetable driver alterations in resected early-stage lung cancer. Transl Lung Cancer Res. 2024 Nov 30;13(11):3096-3105. doi: 10.21037/tlcr-24-433. Epub 2024 Nov 14. PMID: 39670019; PMCID: PMC11632426.
Neuschmid M-C*, Ponholzer F*, Ng C, Maier H, Dejaco H, Lucciarini P, Schneeberger S, Augustin F. Intercostal Catheters Reduce Long-Term Pain and Postoperative Opioid Consumption after VATS. Journal of Clinical Medicine. 2024; 13(10):2842. doi: 10.3390/jcm13102842 *contributed equally
Ponholzer F, Groemer G, Ng C, Maier H, Lucciarini P, Kocher F, Öfner D, Gassner E, Schneeberger S, Augustin F. Sarcopenia and Mediastinal Adipose Tissue as a Prognostic Marker for Short- and Long-Term Outcomes after Primary Surgical Treatment for Lung Cancer. Cancers (Basel). 2023 Nov 30;15(23):5666. doi: 10.3390/cancers15235666
Ponholzer F, Chorazy K, Ng C, Kocher F, Maier H, Lucciarini P, Öfner D, Augustin F. External validation of risk prediction scores in patients undergoing anatomic video-assisted thoracoscopic resection. Surgical Endoscopy. 2023 Apr;37(4):2789-2799. https://doi.org/10.1007/s00464-022-09786-7
Ponholzer F, Ng Caecilia, Maier Herbert, Augustin Florian. Do working hour limitations have an impact on surgical training: a narrative review. AME Surgical Journal. 2023;3:24. https://doi.org/10.21037/asj-22-15
Ponholzer F, Ng C, Maier H, Lucciarini P, Öfner D, Augustin F. Risk factors, complications and costs of prolonged air leak after video-assisted thoracoscopic surgery for primary lung cancer. Journal of Thoracic Disease. 2023. 15(2):866-877. https://doi.org/10.21037/jtd-21-201
Ponholzer F, Schwarz S, Jaksch P, Benazzo A, Kifjak D, Hoetzenecker K, Schweiger T. Duration of extracorporeal life support bridging delineates differences in the outcome between awake and sedated bridge-to-transplant patients. European Journal of Cardio-Thoracic Surgery. 2022. 62(3):ezac363. https://doi.org/10.1093/ejcts/ezac363
Schweiger T, Ponholzer F, Kifjak D, Schwarz S, Benazzo A, Lang G, Tschernko E, Markstaller K, Hoetzenecker K. A Dual-lumen Extracorporal Membrane Oxygenation Cannulation Technique Using a Mobile X-ray Device. The Annals of thoracic surgery. 2022; 30:S0003-4975(22)00661-0. doi: 10.1016/j.athoracsur.2022.04.029
Ponholzer F, Ng C, Maier H, Dejaco H, Schlager A, Lucciarini P, Öfner D, Augustin F. Intercostal Catheters for Postoperative Pain Management in VATS Reduce Opioid Consumption. Journal of Clinical Medicine. 2021; 10(2):372. https://doi.org/10.3390/jcm10020372
Ponholzer F, Kroepfl V, Ng C, Maier H, Kocher F, Lucciarini P, Öfner D, Augustin F. Delay to Surgical Treatment in Lung Cancer Patients and its Impact on Survival in a Video-assisted Thoracoscopic Lobectomy Cohort. Scientific Reports. 2021; 11(1):4914. doi: 10.1038/s41598-021-84162-4
Patents
EP-Patent registration: 23150338.4 (WO2024146932A1): “Fluid and substrate restitution protocol including bile replacement for management of long-term normothermic machine perfusion of livers.“
Selection of Funding
MUI Start (2024)
Title: “Normothermic liver machine perfusion of explanted livers with hepatocellular carcinoma: a novel platform for oncologic assessment and treatment”
Total amount: € 41.049
TWF Tiroler Nachwuchsforscher*innenförderrung (2024)
Title: „The role ofbiiary primary cilia in paediatric liver transplantation”
Total amount: € 37.840
TWF Tiroler Nachwuchsforscher*innenförderrung (2024)
Title: „Precision-cut liver slices as a versatile tool to develop iPSC-based therapies for liver regeneration during normothermic machine perfusion”
Total amount: € 30.8084
TWF Tiroler Nachwuchsforscher*innenförderrung (2024)
Title: „Cytokine absoprtion during prolonged normothermic machine perfusion of porcine livers to modify graft immunogenicity ex vivo”
Total amount: € 37.485
FWF Project MYCOS (2024)
Title: “Antimycotic resistance – Approach from a One “Health Perspective
Total amount: € 90.000
Land Tirol (2024)
Title: „PEAKS – Die Effekte der normothermen Maschinenperfusion auf den Proteinstoffwechsel der Niere“
Total amount: € 118.375
Fa. DEKA Industrial Cooperation Project (2024)
Title: “POD Biological Assessment Study II”
Total amount: € 457.355,06
VASCage GmbH Project, FFG supported (2024)
Title: “High specific gene transfer in ex situ perfused livers to diminish cardiovascular complications in familial hypercholesterolemia”
Total amount: € 1.454.545,45
Chiesi Unrestricted Grant (2024)
Title: “Assessment of the pharmacokinetics and impact of tacrolimus in ex-situ perfused human donor livers: A pilot study”
Total amount: € 15.000
FWF Project P-36922 (2023)
Title: “Malassezia-induced immuno-environment of pancreatic ductal adenocarcinoma – a new player in tumorigenesis and treatment” (Manuel Maglione, Cornelia Speth)
Total amount: € 414.500
Collaborations
- Peter J. Friend, Rutger Ploegh, University of Oxford, Nuffield Department of Surgical Sciences, Oxford, United Kingdom
- Byoung Chol Oh, Johns Hopkins Medical University, Department of Plastic and Reconstructive Surgery, Baltimore, Maryland, USA
- Jerzy Kupiec-Weglinski, University of California Los Angeles (UCLA), Los Angeles, California, USA
- Abdi Reza, Harvard Medical School, Boston, Massachusetts, USA
- Stuart Forbes, Sofia Ferreira Gonzalez, Institute for Regeneration and Repair, Center for Regenerative Medicine, University of Edinburgh, Edingburgh, Scottland
- Emmanuel Morelon, Hospices Civils de Lyon, Hospital Edouard Herriot – Transplantation, néphrologie et immunologie, Lyon, France
- Emmanouil S.Papadakis, Graham Packham, Ramsey Cutress, Cancer Research UK Centre, Cancer Sciences Division, University of Southampton Faculty of Medicine, Southampton General Hospital, Southampton, United Kingdom
- Andrew Cato, Karlsruhe Institute of Technology, Institute of Photon and Synchrotron Radiation, Eggenstein-Leopoldshafen, Germany
- Bruno Podesser, Biocenter, Medical University Vienna, Vienna, Austria
- Stefan Wiese, Faculty for Biology and Biotechnology, Group for Molecular Cell Biology, Ruhr University Bochum, Bochum, Germany