Anichstraße 35
6020 Innsbruck
Fax: +43 (0)50 504 22758
Email: Elke.Gizewski@i-med.ac.at
Website:
Research year
Research Branch (ÖSTAT Classification)
301111, 301401, 302010, 302013, 302043, 302044, 302048, 302055, 302070, 302071, 302074, 302075, 302079, 303039, 305901, 305905
Keywords
Angiography, artificial intelligence, CT, digital imaging, DTI, dual-energy-CT, fMRI, imaging analysis, interventional neuroradiology, interventional oncology, Interventional Radiology, microCT, MR-spectroscopy, MRI, multimodal quantitative MR-imaging, PET- CT, radiation protection, Radiology, Robotics, and ultrasound
Research Focus
- Ultrasound (elastography, musculoskeletal, peripheral nerves, ultrasound guided interventions)
- Multiparametric imaging of prostatic cancer
- MRI (quantification of fat/iron; cardiac MRI; spectrosopy of myocardium; musculoskeletal MRI including stress MRI of the hip and knee, MR mammography, fMRI/VBM, multi-nuclear MRI)
- multimodal, quantitative MRI and artificial intelligence (AI) applications on neuroradiological imaging
- Mikro CT
- CT (cardiac CT, Dual Energy CT, emergency Radiology, trauma, sports injury)
- Interventional Radiology and Neuroradiology (endovascular/oncology), Diagnosis and treatment of HCC (stereotactic RFA, TACE, SIRT)
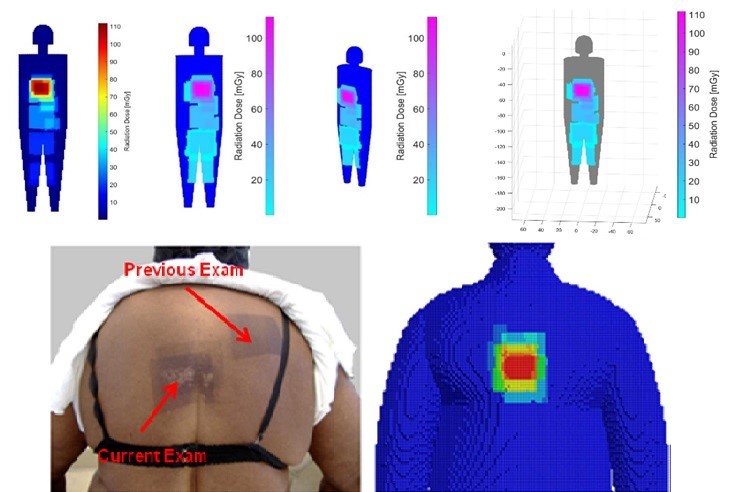
- Real time dose monitoring
- Digital imaging/PACS/postprocessing of imaging data, AI, Radiomics
- Clinical trials with imaging outcome parameters
General Facts
The University Clinic of Radiology has one §98 professorship of Radiology (Univ.-Prof. Dr. Elke R. Gizewski, chair and head of the clinic).
A second §98 professorship “Artificial Intelligence in Radiological Imaging” is currently in the appointment process.
The following research professorships (§99(4)) have been established since 2023:
- Neuroradiology (Univ.-Prof. Dr. Astrid E. Grams)
- Interventional oncology, stereotaxy & robotics (Univ.-Prof. Dr. Reto Bale)
The research focus on “Interventional Radiology” was strengthened in 2024 with a §99(5) professorship (Ass.-Prof. PD Dr. Alexander Loizides)
In 2023, a §99(5) for “Computational Radiology” (Ass.-Prof. Dr. Christoph Birkl) was established.
The department is equipped with state-of-the-art imaging systems for clinical routine and research: seven CT scanners, five MRI scanners (two 3T and three x 1.5T), two PET-CT scanners (in cooperation with the Clinic of Nuclear Medicine), three angiography suites and 15 high-end ultrasound systems. One sliding gantry CT operates in an imaging suite dedicated to stereotaxis and CT-guided procedures. The Radiology Department has been operated fully digitally since 1999 and performs over 300,000 diagnostic and interventional procedures per year. It employs 83 medical staff, including 35 radiologists in training). In total, the Radiology Department provides an excellent basis for speciality training and the teaching of students.
The Experimental and Computational Radiology section (Computational, Experimental) is staffed by eight physicists/mathematicians with different areas of interest, including MRI, image data processing, radiation protection, deep learning and computer applications.
The department accommodates research facilities for animals (high-resolution RF coils for MRI). The Core Facility Micro-CT (Radiologie | Micro-CT) is equipped with two micro-CT scanners (in cooperation with the Department of Orthopaedics and Traumatology) for high-resolution imaging of small animals and one CT for high-resolution scanning of extremities.
The Core Facility for Neuroimaging Research (CF-NIR, Radiologie | Neuroimaging Research) includes a 3T MRI, MR physics, advanced mathematics and artificial intelligence.
Radiological research projects are mostly interdisciplinary with internal and external collaborations. We focus on the rapid translation of research results into clinical practice in diagnostic and interventional Radiology and Neuroradiology.
The Radiology Department has a long-standing PhD programme (Image-Guided Diagnosis & Therapy) and a clinical PhD programme (Clinical Imaging Science). In 2021, the “IGDT” programme (DOC 110-B) received a FWF grant to expand its expertise in mathematics, computer science and engineering. The programme is a partnership between the University of Innsbruck (UIBK) and the Tyrolean Private University (UMIT), with the latter specialising in biomedical engineering, which was transferred to the UIBK in 2024. In 2024, the Clinic of Radiology had ten PhDs, nine clin. PhDs and two Master students associated with one of the 14 radiological research groups.
Research
CT imaging
Lead: PD Dr. Gerlig Widmann
Members: Dr. Anna Luger, Dr. Anna-Katharina Gerstner
a) Head and Neck imaging
- CT comparison of different nasal septal areas between patients with and without nasal obstruction
- Development of a three-dimensional, convolution, deep neural network for distinguishing vital from non-vital persistent cervical lymph nodes in advanced head and neck squamous cell carcinoma after primary concurrent radio-chemotherapy
b) Thoracic imaging
- Tyrolung Lung Health Check Project – AI-based screening of lung cancer, chronic obstructive lung disease (COPD), coronary heart disease (CHD) and digital application-based promotion of public health
- Deep learning-based texture analysis and quantification of fibrosis in systemic sclerosis und rheumatoid arthritis
- Comparison of density-based and texture-based analysis of emphysema in COPD
c) Abdominal imaging
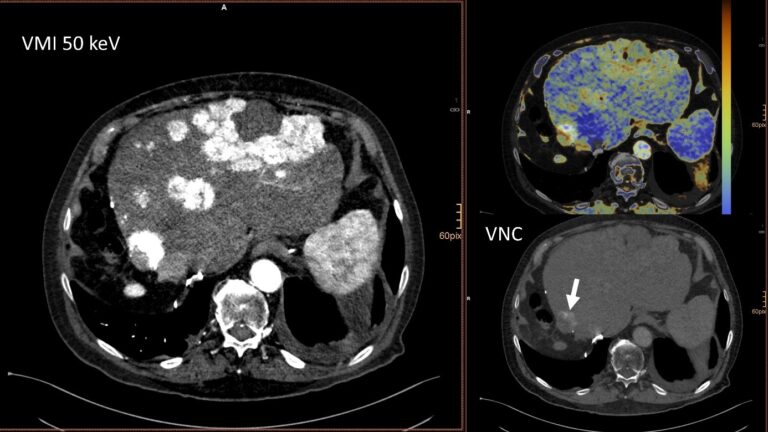
- Dual Energy CT-based evaluation of diffuse liver disease: fibrosis and fat quantification
- Dual Energy CT-based quantification of iron content in liver
- Quantification of hepato cellular carcinoma (HCC) washout and structured reporting of HCC-based on LI-RADS for tumour registry for radiomics research

d) Low dose imaging
- Identification and characterisation of patients being exposed to computed-tomography associated radiation-doses above 100 mSv.
- Development of an ALADA reference quality approach in craniofacial trauma CT
- Clinical verification of an ALADA protocol in craniofacial trauma
- Prediction of ALADA Doses for Implant Site Analysis Using Slope of Hounsfield Units- external collaboration with King Saud University
e) Quality assurance
- Quality assurance in breast imaging project – European Society of Radiology Quality, Safety and Standards Committee, Audit & Standards Subcommittee
Experimental Radiology
a. Image Processing
Lead: PD Dr. Wolfgang Recheis
Image processing and analysis, including rapid prototyping based on radiological data, represent core interests and tasks, including multidimensional visualisation, the quantification of disease patterns based on texture analysis, shape analysis and others. Moreover, our new micro-CT core facility allows depiction of structures on μm scale in all three spatial dimensions.

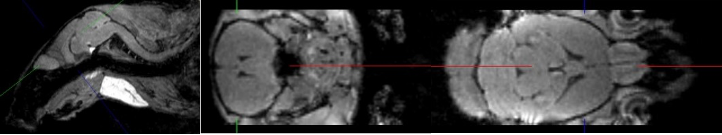
b.Small Animal MRI
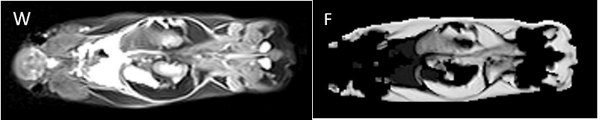
Lead: Dr. Christian Kremser
The Department of Radiology is conducting experimental MR examinations on various animal models and specimens. Over the years, coil setup and imaging sequences have been optimised accordingly. Study topics include mouse spinal cord imaging after shock wave treatment to promote spinal cord repair; volumetry of mouse myocardium to quantify fibrotic changes after constriction of the aorta and pulmonary artery; volumetry of the mouse brain to quantify fixation shrinkage; pulse wave velocity imaging in rabbits to evaluate aortic plaques; volumetric quantification of subcutaneous and visceral fat in mice on different diets; detection of intervertebral disc herniation in knockout mice.
MedCorpInn– Retrospective Intersectional Corpuslinguistic Analysis of Radiological and Medical Reports of Medical University of Innsbruck
Leads: Claudia Posch and Karoline Irschara (University of Innsbruck), Leonhard Gruber and Stephanie Mangesius (Medical University of Innsbruck)
This project is compiling a large linguistic corpus (digitalised data collection) of radiology reports and medical reports. This will allow us to conduct corpus and discourse linguistic as well as gender medicine research. Standardisation, automated data processing and anonymisation mean that the radiology corpus contains over 5 million anonymised radiology reports. These can be queried using corpus linguistic and NLP tools.
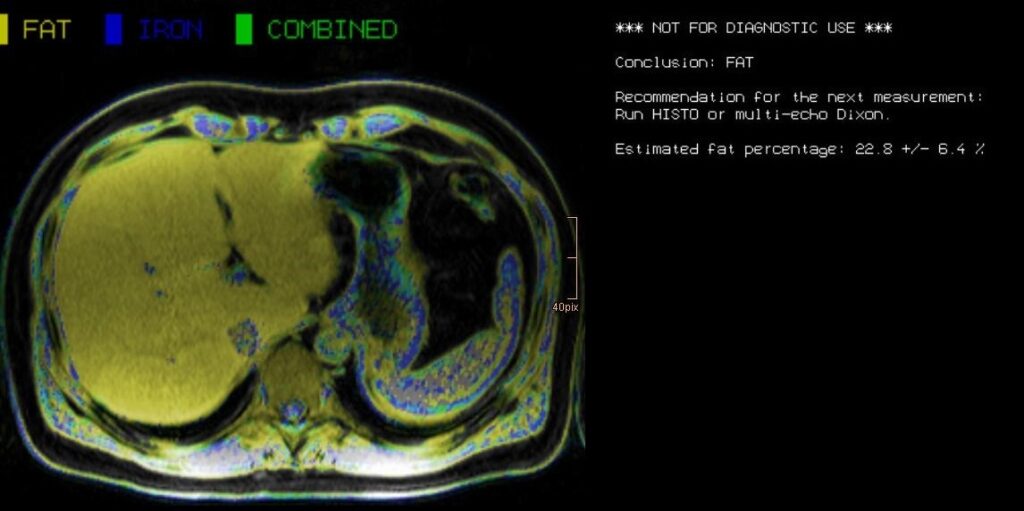
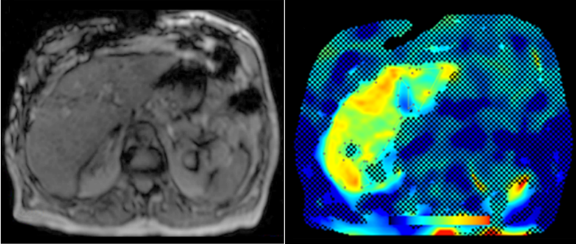
Abdominal MR Imaging
Leads: PD. Dr. Michaela Plaikner, PD. Dr. Benjamin Henninger, Dr. Christian Kremser
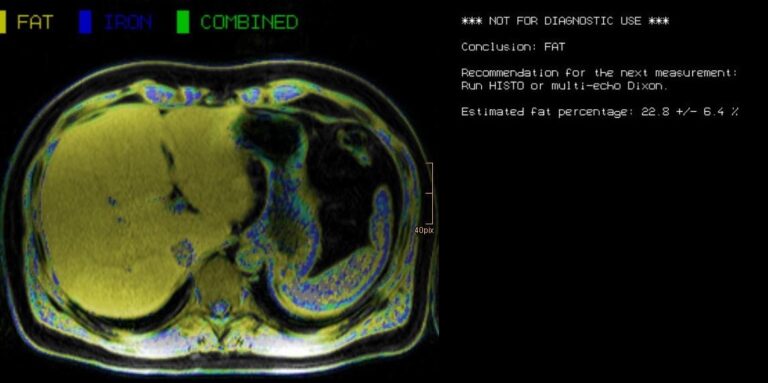
Morphological and functional MRI in all-organ systems development of novel MRI applications and MR sequences. Examples of research projects include fat, iron or combined disease; influence of iron on the evaluation of liver fat (Fig. 6).
a. MRI for the evaluation of diffuse liver disease: evaluation of different MRI methods (relaxometry, chemical shift imaging, multi-echo approach, Dixon screening) to detect diffuse liver disease (fat, iron or combined disease); influence of iron on the evaluation of liver fat (Fig.6).
MR-Elastography (MRE)
MRE is increasingly used in hepatic MRI to detect and classify fibrosis in the early stages before morphological changes have occurred. In our department, MRE is already integrated into the routine hepatic MRI protocol and used for various research projects.
Cardiovascular MR Imaging
Leads: Prof. Dr. Agnes Mayr, Dr. Christian Kremser, Dr. Mathias Pamminger, Dr. Felix Troger, PhD, Matthias Schwab in cooperation with the Department of Cardiology
a. STEMI CMR: CMR Parameters of Myocardial Tissue Damage in ST-Elevation Myocardial Infarction (STEMI).
Since 2005, almost 900 patients have been examined under a comprehensive cardiac MRI (CMR) protocol within the first week as well as 4 months, 12 months and 10 years after acute STEMI. In more than 60 internal original papers, CMR myocardial infarction severity markers and the effects of CMR on optimised risk assessment shortly after STEMI were evaluated.
b. TAVI CMR: CMR to Guide Transcatheter Aortic Valve Implantation (TAVI).
This ongoing randomised study investigates the non-inferiority of TAVI CMR to TAVI CT with regard to efficacy and safety endpoints in the guidance for TAVI evaluation for the first time.
c. 4D Phase Contrast Flow Measurements
- Patients with different grades of aortic valve stenosis: comparison of 4D flow-assessed stenosis severity with 3D echocardiography and invasive measurements.
- Patients with cryptogenic stroke: recording turbulent kinetic energy, changes in flow patterns and regional wall stresses as well as the occurrence of a vortex-shaped flow along the thoracic aortic wall to optimise the elucidation of potential cardioembolic sources.
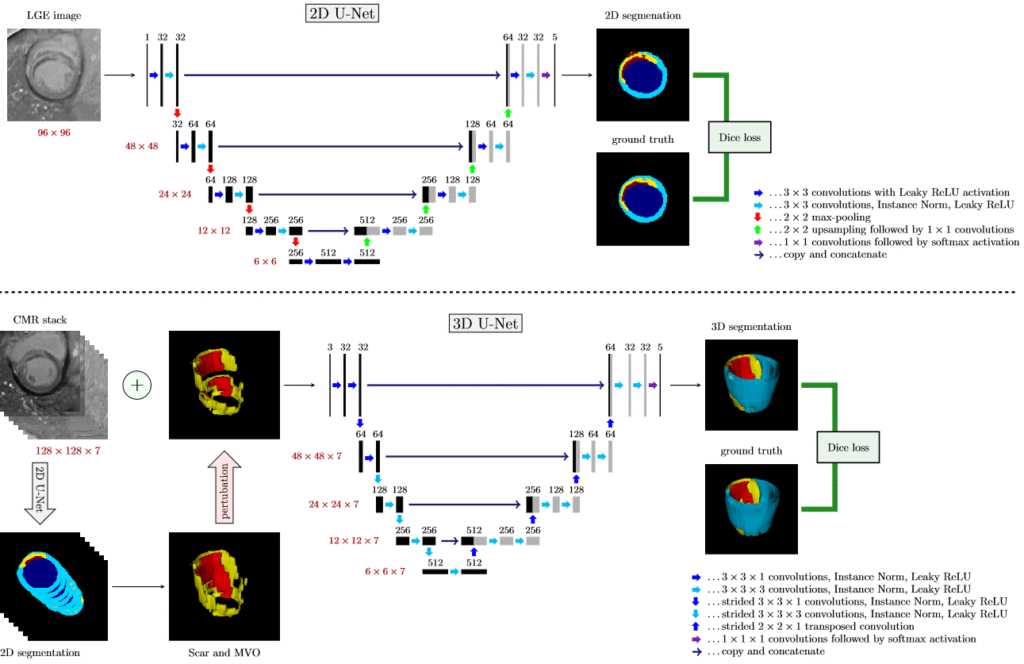
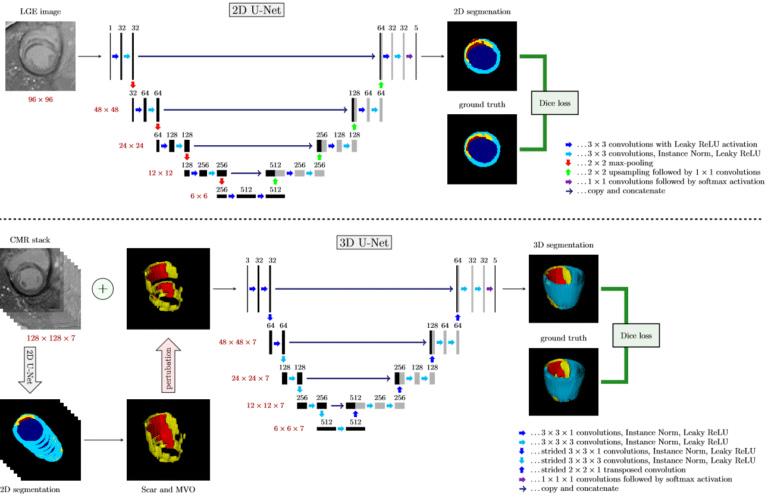
d. Deep learning-based automatic scar segmentation on late enhancement contrast enhanced MR
This ongoing project is developing a fully automatic framework to process 3D cardiac MR datasets for the quantification of infarct scars. First results have already surpassed all state-of-the-art methods.


e. Error correcting 2D-3D cascaded network for myocardial scar segmentation on LGE CMR images
In this work, we develop a cascaded framework of two-dimensional and three-dimensional convolutional neural networks. This pioneering technology enables fully automated calculation of the extent of myocardial infarction.
Musculoskeletal Imaging
Lead: Prof. Dr. Andrea S. Klauser et al., Multicentre collaboration for indication in MSK imaging and interventions
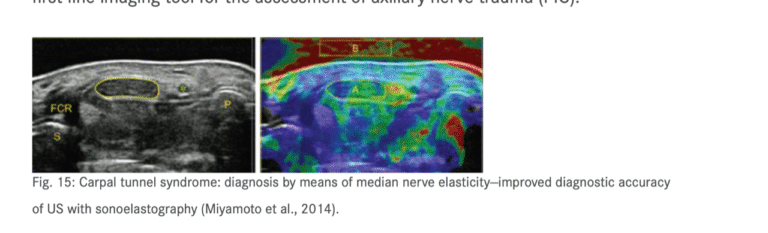
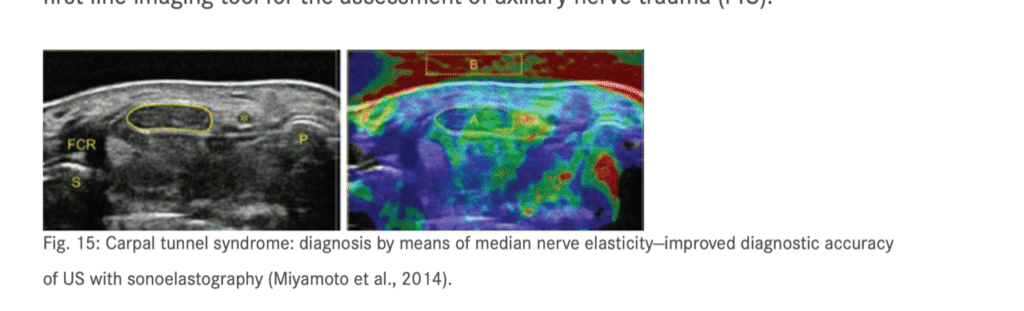
- Sonography of carpal tunnel: definition of cut-off values and correlation with Sonoelastography (Fig. 10) & Sonoelastography of epicondylitis, plantar fasciitis and Achilles tendon: accuracy in comparison with histology
- Sonographically guided (SG) injections in CTS: sonoelastographic appearance
- SG peripheral nerve injection: sonomorphology
- SG nerve entrapment syndromes in comparison with surgical outcome
- SG injection in sacroiliac joints of children: to prove feasibility
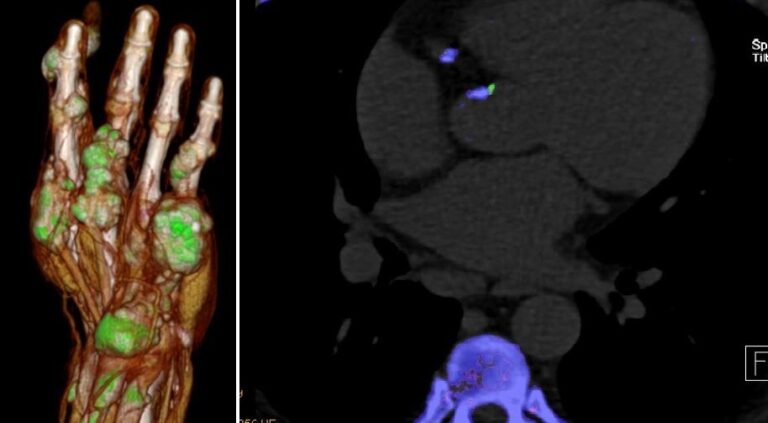
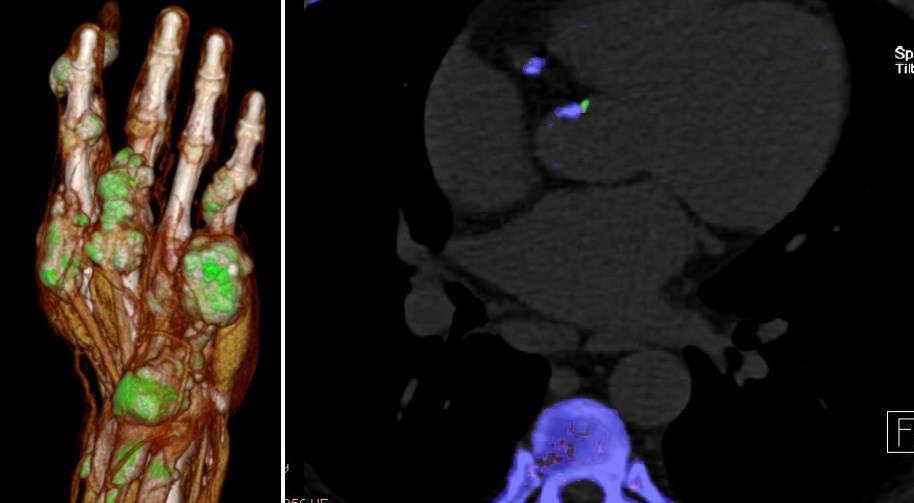
- Dual-energy CT (DECT) in gout: comparison with US-findings, Cardio-DECT in gout and subgroup patients (Fig.11)
- X-ray in comparison with DECT in gout patients
- X-ray in comparison with US in erosion assessment
- MRI in comparison with US in tendon overuse assessment
- MRI whole-spine imaging in inflammatory disease: therapeutic follow-up assessment
- MRI sacroiliitis: therapeutic follow-up assessment
- MR tractography (DTI, ADI) in median nerves of healthy volunteers and CTS patients: comparison with sonography
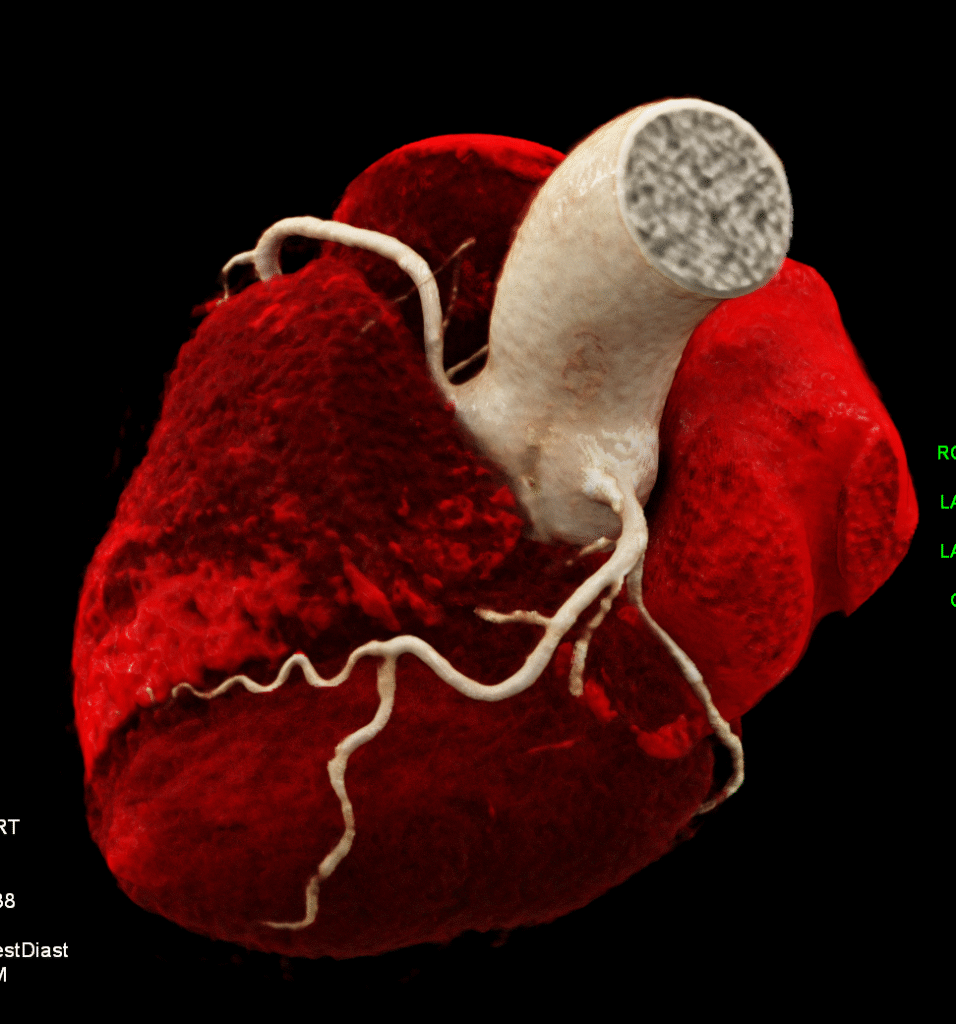
Non-Invasive Cardiac/Cardiovascular CT Imaging
Lead: Prof. Dr. Gudrun Feuchtner, Dr. Pietro G. Lacaita
Our research is focused squarely on two key areas: advanced CT imaging of coronary artery disease and cardiac valves/structural heart disease and novel technologies covering the following topics:
a. Coronary heart disease: atherosclerotic plaque imaging, high-risk plaque marker, the evaluation of novel artificial intelligence (AI) enabled algorithms for quantification of atherosclerosis (Total plaque volume, non-calcified plaque volume, percentage atheroma volume) and machine learning algorithms, peri-coronary and epicardial adipose tissue quantification and breast arterial calcifications for cardiovascular risk stratification and prediction of outcomes; sex-differences and the effect of radiotherapy on coronary arteries.
Our main aim is to evaluate novel CT imaging biomarkers for prediction of CV outcomes, early disease detection and CV risk stratification, with the mission to reduce burden of coronary heart disease. Another focus is sport cardiology and the use of CTA in athletes and CT imaging in preventive cardiology.
Our research team is collaborating with numerous international multicentric consortia (namely: CONFIRM 2: PI Alexander van Rosendael, Leiden Medical University and Ibrahim Danad, Radboud University Medical Centre, Netherlands; and DISCHARGE- extend: Prof Marc Dewey, Charite Berlin) and other US-Universities as part of the CONFIRM2- consortium.
b. Our second focus is the imaging of cardiac valves/endocarditis/structural heart disease by CT for planning TAVR, TMVR and left atrial catheter ablation, imaging of the left atrium including fibrosis mapping, advanced 3D visualisation and congenital heart disease.
c. Novel CT technologies such a Photon Counting CT (installation June 2025) will be a new research focus in the upcoming years.
d. Atherosclerotic Burden and its Relevance to Different Diseases and Treatment Strategies.
Bernhard Glodny, Johannes Petersen
Atherosclerosis can be detected using different diagnostic imaging methods. Treatments are planned using clinical imaging and cardiovascular risk profiles are compiled individually. CT is the most reliable way to quantify the “atherosclerotic burden” of all vascular territories.
It is well established that oral health is linked to overall health. Imaging studies have proven this, showing a clear link between gum inflammation and higher risk of arteriosclerosis. This further confirms the theory that arteriosclerosis is an inflammatory disease.
Ultrasound
Leads: Prof. Dr. Hannes Gruber, PD Dr. Alexander Loizides
- Peripheral nerve sonography
- SG interventions in the peripheral nervous system
- SG carpal tunnel release
- Sonographic evaluation of soft tissue masses (incl. MSK contrast-enhanced sonography (CEUS))
- Sonography of the musculoskeletal system
- Sonographic assessment of functional musculoskeletal disorders
- SG pain therapy
- Angiologic assessment and SG interventions in the vascular system
The surgical ultrasound section is a leader in the development of ultrasound techniques for evaluating peripheral nerves, ultrasound-guided nerve root infiltration and pain therapy. Our work is illustrated in one of the most recent publications.
The axillary nerve (AN) is frequently injured during shoulder trauma and imaging is required to define the site and extent of nerve injury. The AN has a complex course through several soft tissue compartments of the shoulder and axilla. It is vital to have thorough knowledge of the local topography for the detection and sonographic assessment.

Our investigation will define reliable anatomical landmarks for AN sonography in volunteers and validate the proposed sonographic examination protocol in patients. Strict adherence to the proposed examination algorithm made sonography of the AN feasible in all volunteers and patients. The findings correlated well with the gold standard of “surgical exploration” in terms of the severity and topography of neural impairment.
Our study results prove that our algorithm for AN sonography is the best imaging tool for assessing axillary nerve trauma (PIC).
Interventional Oncology/ Stereotaxy and Robotics
Lead: Prof. Dr. Reto Bale
- Image-guided tumour ablation
- Stereotaxy & Robotics
- Targeting & Image Fusion (ablation margin verification)
- Interventional oncology
- Microinvasive Therapy
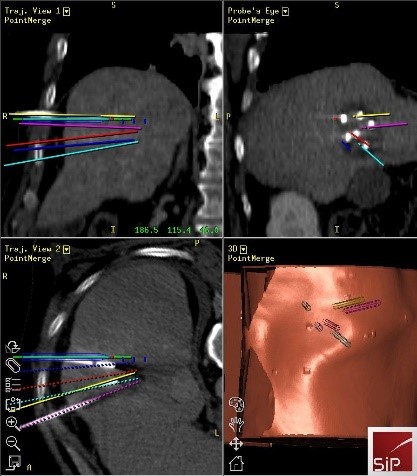
Stereotactic ablation:
Thermal ablation (TA) allows local curative tumour treatment by inducing coagulation necrosis with a high-frequency alternating current. The tumour size is the major limiting factor of conventional US- and CT-guided percutaneous single probe ablation. Navigation systems allow for 3D planning of multiple overlapping ablation zones on the CT datasets and precise transformation into the real patient. We developed the world’s first aiming device for frameless stereotactic punctures in 1995 and performed the first in man stereotactic radiofrequency ablation (SRFA) of a liver tumour in 2001, followed by the first Stereotactic Microwave Ablation (SMWA) in 2008, the first Stereotactic Irreversible Electroporation (SIRE) in 2013 and the first Stereotactic Cryotherapy (SCT).
Meanwhile, our department has successfully treated over 1,500 patients with more than 5,000 liver tumours, most of them being inoperable. Meanwhile, our team has successfully trained the SMZ Ost in Vienna and the Ordensspital Barmherzige Brüder in Linz. In 2023, we conducted the first stereotactic thermal ablation outside Europe under the supervision of Reto Bale (Prof. Odisio at the MD Anderson in Houston, Texas, USA).
Two PhD students from the “Imaged Guided Diagnostics and Therapy – Academic Research Triangle” (IGDT- ART) – funded by the “FWF” program are supervised by Matthias Harders from the LFU and Reto Bale: Adela Moravova: (Semi-)Automatic trajectory planning for multi-probe stereotactic thermal ablation of liver tumours & Stefano Fogarollo: Fast, non-rigid image fusion using deep learning for treatment evaluation after thermal ablation.
Gender imaging
Imaging and Targeted Biopsy of the Genitourinary (GU) Tract
Lead: PD Dr. Friedrich Aigner
- Multiparametric ultrasound of the scrotum
- Multiparametric ultrasound of the prostate
- Multiparametric MRI of the prostate
- Fusion imaging of the GU-tract
- Fusion targeted biopsy of the prostate
- Flow imaging
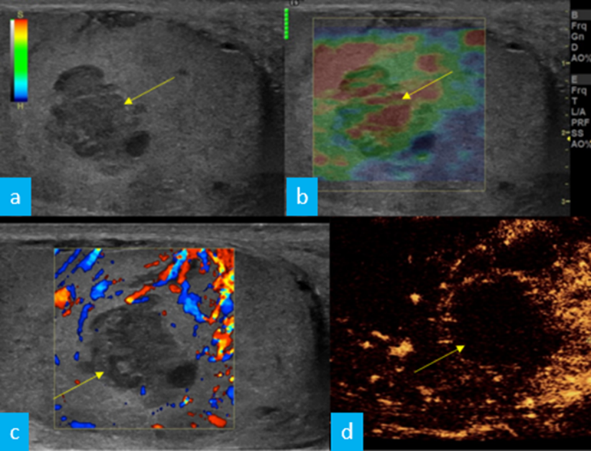
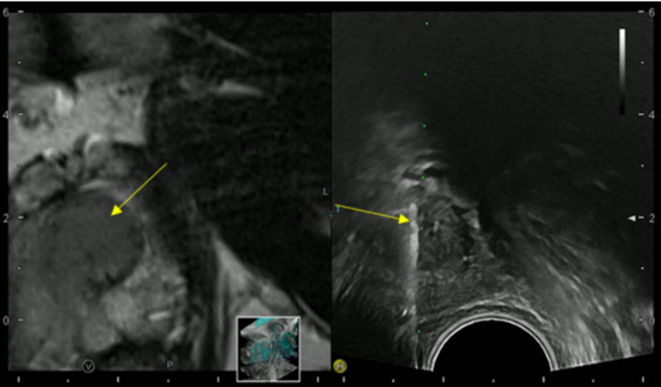
The simultaneous application of structural and functional imaging techniques is described as multiparametric (MP) (Fig. 15/16). Studies have shown that the MP approach results in greater diagnostic accuracy.
The use of fusion imaging in uroradiology improves ultrasound lesion-detection rates, shows more reliable size controls at different time points, is an alternative to in-bore biopsies (Fig. 17) and can be used for focal therapy.
Ultrasound is the imaging tool of choice for assessing flow hemodynamics. Particularly techniques such as Power Doppler Imaging (PDI), B-Flow or Micro Vascular Imaging (MVI, GE Healthcare) can have the potential to replace CEUS for the diagnosis of organ infarctions and the detection of perfusion in lesions with slow blood flow. CEUS is both more invasive and more expensive.

Imaging and Targeted Biopsy of Breast Cancer
Lead: Dr. Birgit Amort, PD Dr. Leonhard Gruber, Dr. Silke Haushammer
The research team specialising in breast cancer diagnosis has extensive experience with all imaging modalities currently used for breast evaluation, including invasive methods such as fine-needle aspirations and/or percutaneous biopsies using stereotaxis or ultrasound guidance. Our unit is the largest screening and assessment centre of the national breast-screening programme in Tyrol. we perform approximately 10,000 mammograms and breast ultrasound studies each year.
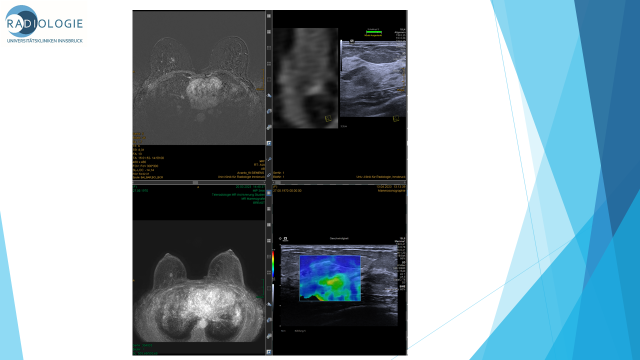
Several new research items have had a significant impact on daily clinical breast diagnostics routines over the past few years: Dual-energy (DE) contrast-enhanced mammography is one of the latest developments in breast care. Imaging with contrast agents in breast cancer has been described in MRI and CT. However, high costs, limited availability and high radiation doses have led to the development of contrast-enhanced spectral mammography (CESM). CESM offers comparable breast cancer detection rates to MRI, yet at a lower false-positive rate, underlining its utility for preoperative local staging. CESM is also an excellent solution for patients with MRI contraindications.
Fusion sonography is now a staple of daily clinical practice, particularly in cases with sonography-occult findings in MRI. It’s value in well-established, as it eliminates the need for costly and stressful MRI biopsies. Our team has the special experience to perform such fusion studies, even using prone-position breast MRI studies by a more localised landmark-based approach.

RVS (Real time virtual sonography) with MRI and CT
- Data Management RVS Bioposy
RVS Biopsy vs. MRI Biopsy similar malignancy rate with 20- 29% (Benchmark: 20-50%)
RVS Biopsy: faster, more economical, more comfortable for the patient
- Advantages RVS I
RVS enables to find most lesions; Short examination time (~ 10 min.); Supine position same as standard examination position in ultrasound; Synchronisation of two modalities in real time
FOV in supine Pos. < in prone Pos.; Biopsy chest wall and axilla near possible
- Advantages RVS II
Biopsy under real time conditions; Selection for MR-biopsies; Significant increase of the detection rate of IELs; Tumour expansion (especially non mass lesions after chemotherapy) more exactly then in B-mode
- Real time ultrasound in Fusions mode- Indications:
Second look-US in incidental enhancing breast lesions (IELs)
Management contrast enhanced lesions/ non mass lesions
NEURORADIOLOGY – DIAGNOSTIC & INTERVENTIONAL
Neuro-Interventions
Retrospective and prospective study of dissecting aneurysms of posterior inferior cerebellar artery (IPICANEMA)
Leads: Prof. Gizewski and Dr. Galijasevic in cooperation with Prof. Wiesmann and Dr. Weyland (University Clinic Aachen)
Dissecting PICA aneurysms are very rare but potentially deadly. They are a complication of a PICA dissection. These aneurysms, although rare, carry a high risk of subarachnoid haemorrhage and subsequent morbidity and mortality. The anatomical variability of the PICA and the complex angioarchitecture of the posterior fossa make both diagnosis and management controversial and insufficiently standardised. The IPICANEMA study combines retrospective and prospective data collection from multiple centres. This identifies the most effective diagnostic strategies, optimal imaging modalities, treatment options (including endovascular and microsurgical approaches) and follow-up protocols. We are particularly focused on outcome measures and complication rates, with the long-term goal of establishing evidence-based guidelines for managing these high-risk patients.
PERForator ANeurysm Registry (PERFAN): a multicentre, exploratory, observational study
Leads: Prof. Gizewski and Dr. Galijasevic in cooperation with PD Dr. Dobrocky (University Hospital Bern)
Perforator aneurysms are rare subtypes of intracranial aneurysms. We need to improve our understanding of the natural history, best management (conservative vs endovascular and surgical) and clinical outcomes in patients with perforator aneurysms because they are rare. Various treatment options have been described, each with its own risks. These must be carefully weighed against the favourable outcomes observed in patients managed conservatively. The the study’s objective is clear: to gain insights into the diagnosis and treatment of perforator aneurysms. This will allow us to define subgroups and specific risk factors for patients with perforator aneurysm. Treatment will prevent clinical deterioration or rebleeding and improve patient care and outcomes.
Aneurysm Wall Enhancement in Cerebral Aneurysms
Leads: Prof. Dr. Grams, Dr. Ladenhauf and Prof. Gizewski in cooperation with PD Dr. Helbok
The objective of this project involving patients with treated or untreated cerebral aneurysms is to investigate aneurysm wall enhancement. We will investigate the presence, frequency and severity of enhancements under different circumstances and their correlation with aneurysm reperfusion.
Evaluation of Device Behaviour and Occlusion Rates in WEB-Treated Aneurysms
Leads: Prof. Dr. Grams and Dr. Galijasevic in cooperation with PD Dr. Bester and Dr. Jungnitz (University Clinic Hamburg)
This study is analysing imaging data from patients treated with the Woven EndoBridge (WEB) device. The aim is to evaluate the influence of device behaviour on aneurysm occlusion rates. We pay particular attention to the alignment between the aneurysm axis and the device, as well as changes in device morphology over time. Imaging projections are limited, so axis alignment is assessed in the working projection when available. Follow-up comparisons rely on standardised projections. We also examine changes in the device’s long axis based on available marker positions and assess occlusion outcomes using a modified Raymond-Roy classification. This study aims to contribute to a better understanding of morphological factors influencing treatment success with the WEB device.
Training in Interventional Radiology – What Can We Learn from Aviation?
Leads: Dr. Ouaret, Prof. Dr. Grams
The introduction of standard procedures and checklists, as well as simulation training, as soon as they became available in the aviation industry in the 1950s and 60s, significantly increased aviation safety. The paradigm shift in medicine is a very slow process. This project’s aim is to explore whether an aviation-style approach to teaching in Interventional Neuroradiology can revolutionise teaching by establishing guidelines for certain procedures and a cockpit simulation training environment.
Outcome after Arterial Punctures: Analysis of the Effectiveness and Safety of Vascular Closure Devices Compared to Manual Compression
Leads: PD Dr. Lukas Lenhart, Prof. Dr. Grams, Prof. Dr. Alexander Loizides, Dr. Maximilian Lutz
This study compares the effectiveness and safety of vascular closure devices with manual compression after arterial punctures in endovascular procedures. Its aim is to assess complications such as bleeding, hematoma and infection through a retrospective analysis of patients over the past 20 years. The study will evaluate outcomes based on patient demographics, medical history, procedure details and post-procedure complications. Using statistical analysis, it determines if vascular closure devices reduce complications compared to manual compression. The goal is to optimise patient care and inform clinical practices. The findings will enhance patient safety and improve medical training by providing evidence-based insights into the advantages of different closure techniques.
Endovascular Thrombectomy for Acute Ischaemic Stroke with Established Large Infarct: multicentre, open-label, randomised trial (TENSION)
Leads: Prof. Gizewski, Prof. Dr. Grams
Members: Dr. Dazinger, Dr. Gindlhuber, Prof. Dr. Glodny, Dr. Galijasevic, in cooperation with Prof. Bendszus (University Clinic Heidelberg) and Prof. Fiehler (University Clinic Hamburg)
The TENSION trial, a multicentre, open-label, randomised study published in The Lancet in October 2023, evaluated the efficacy of endovascular thrombectomy in patients with acute ischemic stroke due to large vessel occlusion and substantial established infarcts (ASPECTS 3–5). The trial proved that thrombectomy significantly improves functional outcomes and reduces mortality at 90 days when compared to medical management alone. Post hoc analyses are underway to further investigate the data and derive additional insights from the study.
“Quantitative Magnetic Resonance Imaging in Patients with Carotid Artery Stenosis before and after Therapy”. QUICAS-study
Leads: Prof. Dr. Grams, Prof. Dr. Christoph Birkl, Dr. Ruth Steiger
Members: Laura Schönherr, PD Dr. Lukas Lenhart, Dr. Malik Galijasevic, PhD, PD Dr. Stephanie Mangesius, PhD, Dr. Hannah Ghazi-Idrissi, in cooperation with Dr. Ingrid Gruber, Prof. Dr. Michael Knoflach, Prof. Dr. Sabine H. Wipper, Prof. Dr. Elke R. Gizewski
Magnetic resonance imaging (MRI) is the only way to acquire quantitative parameters using various sequences. It allows for the depiction of physiological and pathological processes in the brain. Notable sequences include three-dimensional sequences for voxel-based morphometry, diffusion-weighted sequences, arterial spin labeling perfusion, T1 and T2 mapping, multi-echo T2* and MTC sequences, functional (resting state) MRI and phosphorus-based MR spectroscopy. This study focuses on patients with stenoses in the common or internal carotid artery. These patients are scheduled to undergo balloon angioplasty, stent angioplasty or surgical endarterectomy. A study-specific MRI examination is performed. A study-specific neurocognitive assessment and an EEG recording are conducted before and after the therapy. These study-specific measures must be performed 7-0 days prior to therapy, 0-5 days after therapy and about 90 days after therapy. The quantitative MRI data is correlated with the quantitative ultrasound data, neurocognitive data, EEG data, surgery-specific data and other clinical parameters.
Stroke Imaging
31P MRS in Stroke Patients
Leads: Prof. Dr. Grams and Dr. Steiger in cooperation with Prof. Kiechl and Prof. Knoflach
31P MRS is used in patients with acute, subacute and chronic ischemic stroke to gain further insights into the energy metabolism and reorganisation mechanisms of the infarcted brain and surrounding areas during the acute stage and to monitor subacute and chronic changes.
Application of artificial intelligence methods
Leads: Dr. Pereverzyev Jr., PD Dr. Mangesius, PhD, Prof. Dr. Grams, Prof. Dr. Gizewski in cooperation with Dr. Hammerl, Prof. Deisenhammer
In this topic, we will consider the development, adjustment and application of the methods of artificial intelligence (e.g. kernel methods, neural networks, random forests) for predicting clinically relevant information (such as health condition and its future evolution) using radiological information (such as radiological images, various features extracted from the images) and possibly also other available information. The following problems are examined: Prediction of the neurodevelopmental impairments of preterm neonates using characteristics derived from magnetic resonance spectroscopy and diffusion tensor imaging. Prediction of the evolution of multiple sclerosis using planimetric and volumetric characteristics derived from magnetic resonance images. Prediction of the evolution of the infarction from the images of the dual-energy computed tomography.
Dual-Energy CT in Stroke Patients
Leads: Prof. Dr. Grams, Prof. Dr. Gizewski, PD Dr. Mangesius, PhD, Dr. Eisenschink in cooperation with Prof. Kiechl, Prof. Knoflach and Prof. Neumann and Vatankhah Barazandeh (LFU)
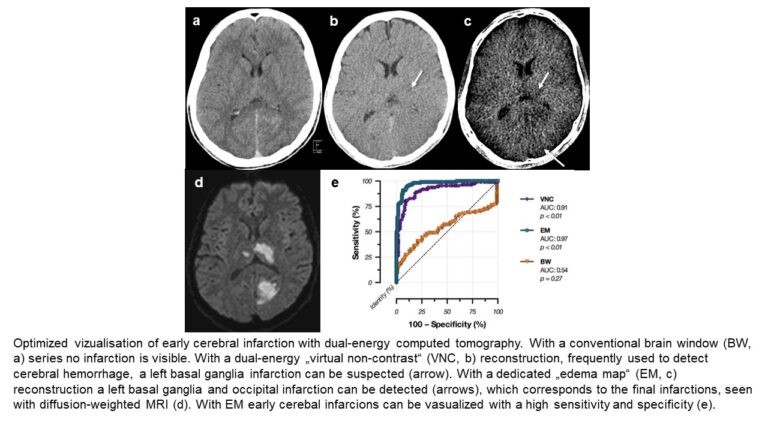
Stroke remains one of the leading causes of death and long-term disability worldwide. Neuroimaging is central to its diagnosis and management. It is vital to detect acute cerebral infarctions early to guide treatment decisions, and dual-energy CT (DECT) has shown proven more sensitive than conventional CT in identifying early infarcts (Fig. 2).
A recent research initiative explores the use of radiomics features from DECT scans acquired post-thrombectomy to predict infarct development before it becomes visually apparent. This method aims to estimate infarct volume and potential clinical outcomes at an early stage. In this context, accurate segmentation of stroke lesions is crucial. The study investigates whether low- and high-energy DECT images, their reconstructed forms, or their combinations can enhance early infarct visibility for machine learning applications. We used co-registered follow-up CTs to define final infarct volume as ground truth. We then trained a self-configuring nnU-Net on multichannel inputs. While automated detection currently does not surpass expert radiological assessment in the earliest stages, it is undoubtedly a supportive diagnostic tool. Fig. 20 (Grams et al. Eur Radiol 2018).
Cerebro-vascular Imaging and Artificial Intelligence
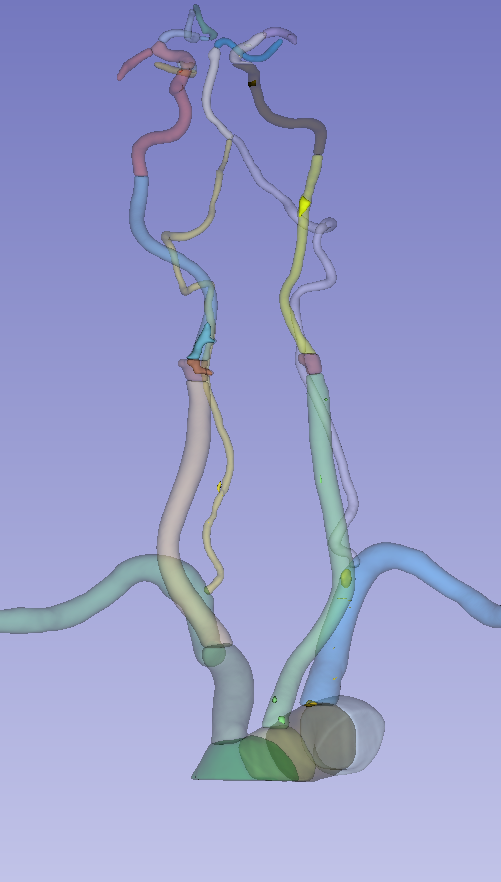
Segmentation and geometrical analysis of the cervical arteries in MRA
Leads: Dr. Pereverzyev Jr., Dr. Mangesius
Members: Dr. Steiger, Dr. Galijasevic, PhD, Prof. Dr. Gizewski in cooperation with Dr. Mayer-Suess, Prof. Knoflach
In this topic, we are developing and applying methodologies for the accurate segmentation and geometrical analysis of the cervical arteries in MRA images. In the development, we are focusing on the reproducibility and a low inter-user variability of the methodology. Fig. 21 provides a clear example of this. Experience will be used for other arteries, organs, structures and imaging modalities.
Deep Learning for automated segmentation of head and neck vasculature and differentiation of lumen and calcified plaque
Leads: Prof. Dr. Gizewski, PD Dr.. Mangesius, Markus Tiefenthaler
Members: Dr. Pereverzyev Jr. in cooperation with Prof. Neumann (LFU)
We developed a novel inference method that preserves vessel continuity by considering the global geometry of vascular structures while reducing the number of high-resolution patches processed. Our approach matches the performance of state-of-the-art methods and can successfully recover missing segments of falsely interrupted arteries. We have extended the method to the entire head and neck arterial tree using data from various MICCAI challenges (AortaSeg24 Challenge [cite imran2025multiclasssegmentationaorticbranches] and TopCoW 2024 Challenge). Next, we will adapt it for MRA data. We can automatically detect calcified plaque within the segmented arteries by leveraging adaptive thresholding. With these foundational steps in an advanced stage, we will use our developed frameworks to extract arterial biomarkers and investigate their role in ischemic stroke incidents.
A PhD student of our IGDT-ART programme is involved in this study and will finish his thesis with this project.
Multi-Class Segmentation of Aortic Branches and Zones in Computed Tomography Angiography: The AortaSeg24 Challenge, Muhammad Imran et al (M. Tiefenthaler, E. Almar-Munoz, M. Schwab) , ArXiv abs/2502.05330 (2025): n. pag.
Neuropediatric imaging and artificial intelligence
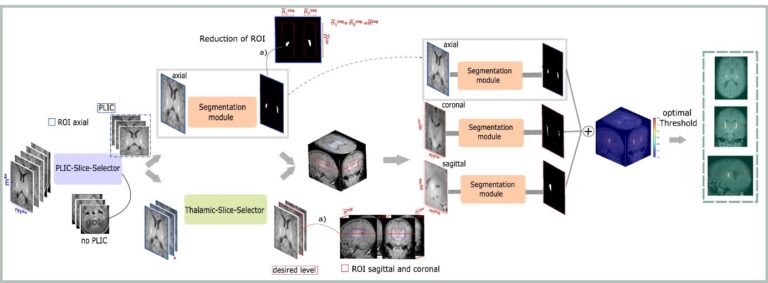
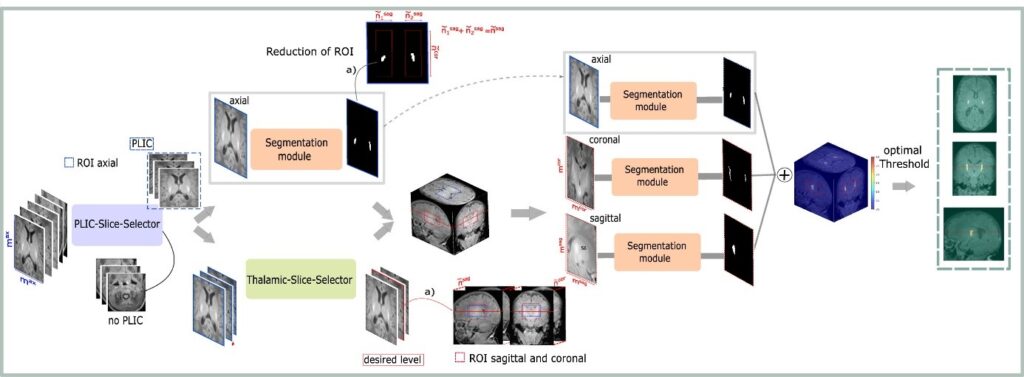
DL for automated segmentation of posterior limb of internal capsule in preterm neonates.
Leads: Univ.-Prof. Dr. Elke Gizewski, Nadja Gruber, PhD, Priv.-Doz. Dr. Stephanie Mangesius, PhD;
Members: Dr. Malik Galijasevic, PhD and Prof. Dr. Birkl in cooperation with Prof. Kiechl-Kohlendorfer, Dr. Neubauer and Dr. Hammerl (Department for Neonatology)
Segmenting specific brain tissue from MRI volumes is vital for brain disease diagnosis, progression assessment and monitoring of neurological conditions. We address the problem of segmentation of the posterior limb of internal capsule (PLIC) in preterm neonates. We propose a CNN-based pipeline comprised of slice-selection modules and a multi-view segmentation model. This exploits the 3D information contained in the MRI volumes to improve segmentation performance. Standard evaluation metrics and expert assessments confirm the good performance of the proposed framework, with the latter being more relevant for clinical applicability.
Advanced imaging techniques in preterm neonates
Leads: PD Dr. Stephanie Mangesius, Prof. Dr. Elke Gizewski
Members: PhD, Dr. Birkl, Dr. Anna Katharina Stock, PhD; Prof. Dr. Astrid Grams; Marie-Christin Pali, PhD, and in cooperation with Prof. Kiechl-Kohlendorfer, Dr. Neubauer and Dr. Hammerl (Department for Neonatology)
Due to advances in neonatal care, survival rates for very preterm infants have been successfully boosted, with over 95% surviving <32 weeks gestation in Tyrol. However, these infants remain at high risk of adverse motor and cognitive outcomes. While MRI-detected brain injuries correlate with development, predictive accuracy for individual outcomes remains limited. This highlights the need for additional imaging markers and advanced neuroimaging techniques to improve early risk identification.
In this project, we collect various MR imaging biomarkers, including advanced quantitative sequences around the estimated date of birth. We then apply deep learning-based methods to estimate the prognosis of preterm infants’ development.
We have also established cooperation arrangements with the children’s hospital Zurich, including foetal imaging and outcome predictions in children with malformations.
Quantitative imaging biomarkers in neurodegenerative diseases
Leads: PD Dr. Stephanie Mangesius, PhD, Dr.. Anna Katharina Stock, PhD; Dr. Sergiy Pereverzyev Jr. in cooperation with the Department of Neurology
This project aims to investigate the clinical value of quantitative imaging biomarkers and novel imaging methods, as well as image post-processing techniques, in various neurodegenerative diseases such as Parkinson’s disease, dementia and multiple sclerosis.
Comparison of software applications
Lead: PD Dr. Mangesius, PhD
Members: Prof. Dr. Gizewski, Dr. Lenhart, PhD, Dr. Stock, PhD, Dr. Steiger
The advance of precision medicine has led to the development of numerous open source and commercial software applications that allow fast automated and unbiased measurement of brain volumes. To date, none of these approaches has yet emerged as a gold standard in clinical routine or research. Measuring atrophy in routine clinical practice is an unmet need. While these applications are highly consistent within themselves, consistency has not been as clearly demonstrated when they are compared to each other. This point is crucial for consistency across clinical care providers and research groups in the search for imaging markers. The present study quantifies the agreement across different software applications for different neurological diseases with degenerative aspects.
Our study on subjects with cognitive deterioration and hippocampal atrophy and gender- and age-adjusted healthy controls clearly identified significant and clinically relevant differences. This highlights the need for standardised assessment and shows that the inconsistent use of software tools in the work-up of dementia must be avoided. Automated evaluation of brain and lesion volume is essential in multiple sclerosis imaging to monitor treatment efficacy and serve as a reliable outcome measure. We also aim to evaluate the consistency of various software solutions within this population, given the young age of many patients and their likely transitions between radiology centres over time.
MR planimetric measurements for diagnosis and outcome prediction of Multiple Sclerosis
Lead: PD Dr. Mangesius, PhD
Members: Prof. Dr. Gizewski and Dr. Pereverzyev Jr. in cooperation with Prof. Deisenhammer (Neurology Innsbruck)
The advent of MRI has provided a powerful tool for monitoring the dynamics of pathological changes in multiple sclerosis. However, conventional approaches offer only limited, often subjective information that is directly relevant to clinical progression. Continued developments of imaging methods and their use for diagnosis, monitoring pathology and understanding disease progression are of interest. The main objective of this study is therefore to investigate whether the simple and easily applicable MR planimetry can predict the technically more complex volumetric measurements at baseline and at follow-up examinations. In a follow-up study, we applied feature selection to classify disability in multiple sclerosis using MR-based planimetric and volumetric measurements. Planimetric features enabled high-accuracy classification of disease severity. Notably, classifiers using a reduced set of these features performed as well or better than those using larger variable sets, highlighting a clinically feasible subset of measurements for distinguishing between less- and more-severe MS courses.
Combining Liquor Data and Radiomics for insights in Multiple Sclerosis
Leads: Prof. Dr. Gizewski, PD Dr. Mangesius, PhD, Marie-Chrstin Pali, PhD, Markus Tiefenthaler in cooperation with Prof. Neumann (LFU) and Dr. Hegen (Neuroimmunologie)
We aim to bridge the gap between cerebrospinal fluid analysis and multimodal imaging by using radiomics to quantitatively assess imaging features across multiple MRI sequences. Key biomarkers, such as lesion count and volume, will be extracted and integrated with radiomic features. This approach aims to improve the understanding of disease-related imaging biomarkers and their correlation with clinical and medical data.
Quantitative MRI Parameter Assessment in Idiopathic Intracranial Hypertension:
Lead: Dr. Lukas Lenhart, PhD Florian Frank
By analysing quantitative MRI parameters such as venous sinus stenosis or tortuous emissary veins as well as other parameters (e.g., empty sella, prominent optic nerve sheaths), this study aims to determine if the diagnosis of idiopathic intracranial hypertension (IIH) can be predicted.
Analysis of the Longitudinal grey and white matter changes in adolescents:
Leads: Dr. Lukas Lenhart, PhD; in cooperation with Dr. Manuela Gander, Prof. Dr. Elke Gizewski
Using voxel-based morphometry, a well-established method for segmenting the whole brain, this study investigates quantitative and functional associations with grey and white matter in adolescents with personality disorders.
Quantitative Neuro-MRI
Anisotropy and field strength dependence of relaxation rates in single and crossing fibre white matter
Lead: Prof. Dr. Christoph Birkl
Members: Dr. Melanie Bauer, Dr. Christian Kremser, Prof. Dr. Elke Ruth Gizewski, Dr. Claudia Lenz,
MRI parameters depend on the orientation of white matter fibres relative to the main magnetic field. However, the impacts of fibre complexity and field strength remain unclear. Therefore, in this study, we examine the fibre orientation dependence of R2, R2* and R2’ as well as their field strength-dependent and -independent components in single and crossing fibre voxels of brain white matter at 1.5 T and 3 T.
Influence of tissue anisotropy in quantitative brain MRI
Leads: Prof. Dr. Christoph Birkl, Dr. Melanie Bauer, Prof. Dr. Elke R. Gizewski
MRI images of the brain are influenced by the orientation of nerve fibres relative to the MRI’s magnetic field. This direction-dependent effect, known as anisotropy, can mimic disease-related changes in MRI. Unfortunately, our understanding of how tissue composition and anisotropy influence quantitative MRI is limited. This lack of knowledge has become a major problem in the clinical application of quantitative MRI. The aim of this project is to combine various investigations, such as quantitative MRI post-mortem and in vivo, as well as histological and biochemical analyses, to uncover the origins of anisotropy in quantitative MRI and pave the way for its clinical application.
Biophysical Modeling for Microstructural Iron Quantification
Lead: Prof. Dr. Christoph Birkl, PhD student: Alexander Stürz,
Quantitative MRI facilitates the non-invasive investigation of microstructural tissue components. Magnetisable trace elements, such as iron in its various binding forms, sizes and concentrations, induce local magnetic field inhomogeneities, imprinting distinct signatures on the NMR signal. Reconstructing and characterising these iron sources remains challenging due to the constraints of finite resolution and the inherently ill-posed nature of the problem. To precisely evaluate microstructural iron composition, advanced biophysical models are needed which extend beyond traditional quantitative MRI biomarkers such as QSM and R2*.
Experiments, including phantom studies and in vivo measurements in both healthy and pathological brain tissue, have been conducted to analyse NMR signal composition at 1.5T and 3T. Initial results are promising, laying the foundation for an improved model of iron source separation.
Quantitative MRI in brain tissue with extreme iron overload
Leads: Prof. Christoph Birkl, Prof. Elke Gizewski, Prof. Bernhard Glodny, Dr. Marlene Panzer, Prof. Heinz Zoller
This project focuses on the quantification of iron content in brain tissue with an extreme iron overload, such as in patients with aceruloplasminemia. One endeavour is to compare various algorithms for R2* mapping and Quantitative Susceptibility Mapping in situations with extreme iron deposits. The aim is to determine how such extreme iron deposits can best be measured using quantitative MRI.
Neuro-oncological Imaging
Transforming Brain Tumour Care: Advanced Imaging for Monitoring Radiotherapy Response
Leads: PD Dr. Dr. Mangesius, PhD, Prof. Dr. Birkl and Prof. Dr. Gizewski, in cooperation with Prof. Ganswindt and Dr. Mangesius (Radiooncology Innsbruck), PD Freyschlag, Dr. Kerschbaumer, Dr. Pinggera and Prof. Thomé (Neurosurgery Innsbruck), Prof. Virgolini (Nuclear Medicine Innsbruck) and Prof. Wöhrer (Neuropathology Innsbruck)
Assessing treatment response after radiotherapy for brain metastases and primary tumours remains challenging, even with advanced imaging. Differentiating true tumour progression from treatment-related changes such as radiation necrosis or pseudo-progression is critical for timely and appropriate management but often requires invasive biopsy. This study aims to establish a local, quantitative image analysis pipeline to improve the early, non-invasive detection of treatment response. Additionally, it investigates the impact of tumours and therapy on normal-appearing white matter to better predict outcomes. These efforts seek to support individualised treatment decisions, improve diagnostic accuracy and ultimately enhance patient prognosis and quality of life.
Advanced diffusion MRI of brain tumour patients
Leads: Dr. Melanie Bauer (Postdoc.Mobility Fellow), PD Dr. Stephanie Mangesius, PhD, Prof. Dr. Christoph Birkl in cooperation with Department of Neurosurgery
The advanced diffusion model neurite orientation dispersion and density imaging (NODDI) allows the differentiation of microstructural compartments within one voxel. The aim of this study is to improve the diagnosis of brain tumours using NODDI. A fully automatic segmentation method of healthy, oedematous and tumour tissue will be the basis to distinguish between glioma and metastasis , as well as between low and high grade glioma.
Quantitative MRI parameters in normal appearing contralateral tissue of glioblastoma patients are associated with survival
Leads: PD Dr. Stephanie Mangesius, Prof. Christoph Birkl
Members: Alberto Galimberti, Prof. Dr. Elke R. Gizewski in cooperation with Dr. Julian Mangesius, Dr. Johannes Kerschbaumer, Prof. Christian Freyschlag, Prof. Ute Ganswindt,
Glioblastoma patients often develop tumour recurrence in the contralateral hemisphere, far from the initial tumoral site, even after complete resection, contributing to the poor survival rates. Longitudinal relaxation rate (R1) and effective transverse relaxation rate (R2*) mapping are quantitative MRI techniques that allows characterisation of tissue composition in vivo. In brain tissue, R1 and R2* are primarily affected by iron and myelin content. A recent relaxivity model (R1-R2* relaxivity) has been proposed as a marker of iron homeostasis. Aim of this study was to explore the association with patients’ survival of R1, R2* and R1-R2* in different contratumoural brain regions before surgery.
Optimising MRI Protocols for Brain Radiosurgery
Leds: PD Dr. Mangesius, PhD and Prof. Dr. Gizewski in cooperation with Prof. Ganswindt and Dr. Julian Mangesius (Radiooncology Innsbruck).
Accurate delineation of the target volume is vital for effective stereotactic radiotherapy (SRT) of brain metastases. This study examined the impact of MRI sequence and timing after contrast agent (CA) administration on lesion volume measurements. Different sequences and imaging delays were found to have a significant influence on apparent volumes, with notable variability in small lesions due to differences in border definition. Volume tended to increase with time post-CA, regardless of sequence. These findings highlight the importance of standardised imaging protocols to reduce variability, improve lesion detectability and ensure consistent, precise treatment planning in SRT. Optimisation of MRI timing and sequence selection is essential for accurate radiotherapy targeting.
Pictures
Selected Publications
CT Imaging
- Widmann G, Luger AK, Sonnweber T, Schwabl C, Cima K, Gerstner AK, Pizzini A, Sahanic S, Boehm A, Coen M, Wöll E, Weiss G, Kirchmair R, Gruber L, Feuchtner GM, Tancevski I, Löffler-Ragg J, Tymoszuk P. Machine Learning Based Multi-Parameter Modeling for Prediction of Post-Inflammatory Lung Changes. Diagnostics (Basel). 2025 Mar 20;15(6):783. doi: 10.3390/diagnostics15060783
- Santer M, Zelger P, Schmutzhard J, Freysinger W, Runge A, Gottfried TM, Tröger A, Vorbach S, Mangesius J, Widmann G, Graf S, Hofauer BG, Dejaco D. The Neck-Persistency-Net: a three-dimensional, convolution, deep neural network aids in distinguishing vital from non-vital persistent cervical lymph nodes in advanced head and neck squamous cell carcinoma after primary concurrent radiochemotherapy. Eur Arch Otorhinolaryngol. 2024 Nov;281(11):5971-5982. doi: 10.1007/s00405-024-08842-3. Epub 2024 Jul 30. PMID: 39078472; PMCID: PMC11512899.
- Heppt H, Widmann G, Riechelmann F, Runge A, Riechelmann H, Giotakis AI. CT comparison of the nasal airway anterior and posterior to the piriform aperture in patients with and without nasal obstruction. Head Face Med. 2024 Mar 27;20(1):20. doi: 10.1186/s13005-024-00420-6. PMID: 38532483; PMCID: PMC10967109.
- Santer M, Riechelmann H, Hofauer B, Schmutzhard J, Freysinger W, Runge A, Gottfried TM, Zelger P, Widmann G, Kranebitter H, Mangesius S, Mangesius J, Kocher F, Dejaco D. Radiomic Assessment of Radiation-Induced Alterations of Skeletal Muscle Composition in Head and Neck Squamous Cell Carcinoma within the Currently Clinically Defined Optimal Time Window for Salvage Surgery-A Pilot Study. Cancers (Basel). 2023 Sep 20;15(18):4650. doi: 10.3390/cancers15184650. PMID: 37760620; PMCID: PMC10527389.
Experimental Radiology
- Gollmann-Tepeköylü C, Nägele F, Graber M, Pölzl L, Lobenwein D, Hirsch J, An A, Irschick R, Röhrs B, Kremser C, Hackl H, Huber R, Venezia S, Hercher D, Fritsch H, Bonaros N, Stefanova N, Tancevski I, Meyer D, Grimm M, Holfeld J.: Shock waves promote spinal cord repair via TLR3. JCI Insight. 2020; 5(15): e134552.
- García-Martínez, D., Bastir, M., Villa, C. Daniel García-Martínez, Markus Bastir, Chiara Villa, Francisco García-Río, Isabel Torres-Sánchez, Wolfgang Recheis, Alon Barash, Roman Hossein Khonsari, Paul O’Higgins, Marc R. Meyer & Yann Heuzé.: Late subadult ontogeny and adult aging of the human thorax reveals divergent growth trajectories between sexes. Sci Rep 2020, Jul 1;10(1):10737.
- Radlinger B, Ress C, Folie S, Salzmann K, Lechuga A, Weiss B, Salvenmoser W, Graber M, Hirsch J, Holfeld J, Kremser C, Moser P, Staudacher G, Jelenik T, Roden M, Tilg H, Kaser S. Empagliflozin protects mice against diet-induced obesity, insulin resistance and hepatic steatosis. Diabetologia. 2022 Dec 16. doi: 10.1007/s00125-022-05851-x. Epub ahead of print. PMID: 36525084.
- Unterberger, S.H.; Berger, C.; Schirmer, M.; Pallua, A.K.; Zelger, B.; Schäfer, G.; Kremser, C.; Degenhart, G.; Spiegl, H.; Erler, S.; et al. Morphological and Tissue Characterization with 3D Reconstruction of a 350-Year-Old Austrian Ardea purpurea Glacier Mummy. Biology 2023, 12, 114. https://doi.org/10.3390/biology12010114
- Gizewski ER, Verius M, Rehani MM, Jaschke W. Cumulative Effective Dose During Fluoroscopically Guided Interventions (FGI): Analysis of More Than 5000 FGIs in a Single European Center. Cardiovasc Intervent Radiol. 2024 Jan;47(1):101-108. doi: 10.1007/s00270-023-03604-w.
- Angermann, C., Bereiter-Payr, J., Stock, K., Degenhart, G.#, & Haltmeier, M.. Three-Dimensional Bone-Image Synthesis with Generative Adversarial Networks. Journal of Imaging, 2024. 10(12), 318.
Abdominal MR-Imaging
- Henninger B, Alustiza J, Garbowski M, Gandon Y.: Practical guide to quantification of hepatic iron with MRI. Eur Radiol. 2020 Jan;30(1):383-393. doi: 10.1007/s00330-019-06380-9.
- Henninger B, Plaikner M, Zoller H, Viveiros A, Kannengiesser S, Jaschke W, Kremser C.: Performance of different Dixon-based methods for MR liver iron assessment in comparison to a biopsy-validated R2* relaxometry method. Eur Radiol. 2020 Sep 23. doi: 10.1007/s00330-020-07291-w. Online ahead of print.
- 5-T MR relaxometry in quantifying splenic and pancreatic iron: retrospective comparison of a commercial 3D-Dixon sequence and an established 2D multi-gradient echo sequence. Plaikner M, Lanser L, Kremser C, Weiss G, Henninger B. Eur Radiol. 2023 Feb 17. doi: 10.1007/s00330-023-09451-0. Online ahead of print. PMID: 36800012
- Tissue iron distribution in patients with anemia of inflammation: results of a pilot study. Lanser L, Plaikner M, Schroll A, Burkert FR, Seiwald S, Fauser J, Petzer V, Bellmann-Weiler R, Fritsche G, Tancevski I, Duftner C, Pircher A, Seeber A, Zoller H, Kremser C, Henninger B, Weiss G. Am J Hematol. 2023 Jun;98(6):890-899. doi: 10.1002/ajh.26909. Epub 2023 Mar 15. PMID: 36880875.
Cardiovascular MR-Imaging
- Poskaite P, Kremser C, Pamminger M, Troger F, Reiter G, Reinstadler SJ, Metzler B, Rehwald WG, Kim RJ, Mayr A. Magnetization-transfer flow-independent dark-blood delayed enhancement cardiac MRI optimizes discrimination of ST-elevation myocardial infarct borders. Eur Radiol. 2024 Dec 5. doi: 10.1007/s00330-024-11192-7.
- Troger F, Klug G, Poskaite P, Tiller C, Lechner I, Reindl M, Holzknecht M, Fink P, Brunnauer EM, Gizewski ER, Metzler B, Reinstadler S, Mayr A. Mitral annular disjunction in out-of-hospital cardiac arrest patients-a retrospective cardiac MRI study. Clin Res Cardiol. 2024 May;113(5):770-780.
- Reindl M, Lechner I, Holzknecht M, Tiller C, Fink P, Oberhollenzer F, von der Emde S, Pamminger M, Troger F, Kremser C, Laßnig E, Danninger K, Binder RK, Ulmer H, Brenner C, Klug G, Bauer A, Metzler B, Mayr A*, Reinstadler SJ*. Cardiac Magnetic Resonance Imaging Versus Computed Tomography to Guide Transcatheter Aortic Valve Replacement: A Randomized, Open-Label, Noninferiority Trial. Circulation. 2023 Oct 17;148(16):1220-1230.
- Pamminger M, Reindl M, Kranewitter C, Troger F, Tiller C, Holzknecht M, Lechner I, Poskaite P, Klug G, Kremser C, Reinstadler SJ, Metzler B, Mayr A. Prognostic value of pulmonary transit time by cardiac magnetic resonance imaging in ST-elevation myocardial infarction. Eur Radiol. 2023 Feb;33(2):1219-1228.
- Troger F, Tiller C, Reindl M, Lechner I, Holzknecht M, Pamminger M, Poskaite P, Kremser C, Ulmer H, Gizewski ER, Bauer A, Reinstadler S, Metzler B, Klug G, Mayr A. Slice positioning in phase-contrast MRI impacts aortic stenosis assessment. Eur J Radiol. 2023 Feb 1;161:110722.
Musculoskeletal Imaging
- Held J, Haschka D, Lacaita PG, Feuchtner GM, Klotz W, Stofferin H, Duftner C, Weiss G, Klauser AS. Review: The Role of Dual-Energy Computed Tomography in Detecting Monosodium Urate Deposits in Vascular Tissues. Curr Rheumatol Rep. 2024 Aug;26(8):302-310. doi: 10.1007/s11926-024-01151-y
- Sconfienza LM, Adriaensen M, Albano D, Allen G, Aparisi Gómez MP, Bazzocchi A, Beggs I, Bignotti B, Chianca V, Corazza A, Dalili D, De Dea M, Del Cura JL, Di Pietto F, Drakonaki E, Facal de Castro F, Filippiadis D, Gielen J, Gitto S, Gupta H, Klauser AS, Lalam R, Martin S, Martinoli C, Mauri G, McCarthy C, McNally E, Melaki K, Messina C, Mirón Mombiela R, Neubauer B, Olchowy C, Orlandi D, Plagou A, Prada Gonzalez R, Rutkauskas S, Snoj Z, Tagliafico AS, Talaska A, Vasilevska-Nikodinovska V, Vucetic J, Wilson D, Zaottini F, Zappia M, Obradov M.: Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part I, shoulder. Eur Radiol. 2020 Feb;30(2):903-913.
- Gruber, L., Kremser, C., Zelger, B., Schwabegger, A., Josip, E., Dammerer, D., Thaler, M., Henninger, B. Evaluation of Classic and Quantitative Imaging Features in the Differentiation of Benign and Atypical Lipomatous Soft Tissue Tumors Using a Standardized Multiparametric MRI Protocol: A Prospective Single-Centre Study in 45 Patients. Curr. Oncol. 2023, 30, 3315–3328. https://doi.org/10.3390/curroncol30030252
Imaging and Targeted Biopsy of the Genitourinary (GU) Tract
- Steinkohl F, Luger AK, Gruber L, Pichler R, Heidegger I, Bektic J, Aigner F. Patients’ anxieties and fears: a comparison between transrectal prostate biopsy and prostate MRI. Transl Androl Urol. 2024 Oct 31;13(10):2201-2208. doi: 10.21037/tau-24-239. Epub 2024 Oct 28. PMID: 39507871
- Heidegger I, Frantzi M, Salcher S, Tymoszuk P, Martowicz A, Gomez-Gomez E, Blanca A, Lendinez Cano G, Latosinska A, Mischak H, Vlahou A, Langer C, Aigner F, Puhr M, Krogsdam A, Trajanoski Z, Wolf D, Pircher A. Prediction of Clinically Significant Prostate Cancer by a Specific Collagen-related Transcriptome, Proteome, and Urinome Signature. Eur Urol Oncol. 2024 Jun 7:S2588-9311(24)00144-5. doi: 10.1016/j.euo.2024.05.014. Online ahead of print. PMID: 38851995
- Artamonova N, Djanani A, Schmiederer A, Pipp I, Compérat E, di Santo G, Aigner F, von der Heidt A, Heidegger I. Small cell neuroendocrine prostate cancer with adenocarcinoma components-case report and literature review. Transl Androl Urol. 2024 May 31;13(5):868-878. doi: 10.21037/tau-23-541. Epub 2024 May 27. PMID: 38855597
Imaging and Targeted Biopsy of Breast Cancer
- Kremser C, Gruber L, Dietzel M, Amort B, Santner W, Daniaux M. Quantification of breast biopsy clip marker on routine breast MRI sequences: a phantom study. Eur Radiol Exp. 2024 Nov 15;8(1):128. doi: 10.1186/s41747-024-00525-2.
- Daniaux M, Gruber L, De Zordo T, Geiger-Gritsch S, Amort B, Santner W, Egle D, Baltzer PAT. Preoperative staging by multimodal imaging in newly diagnosed breast cancer: Diagnostic performance of contrast-enhanced spectral mammography compared to conventional mammography, ultrasound, and MRI. Eur J Radiol. 2023 Jun;163:110838. doi: 10.1016/j.ejrad.2023.110838. Epub 2023 Apr 15.PMID: 37080064
- Daniaux M, Gruber L, Santner W, Czech T, Knapp R. Interval breast cancer: Analysis of occurrence, subtypes and implications for breast cancer screening in a model region. Eur J Radiol. 2021 Oct;143:109905. doi: 10.1016/j.ejrad.2021.109905. Epub 2021 Aug 10.PMID: 34403883
Non-invasive Cardiac/Cardiovascular CT-Imaging
- Feuchtner GM, Barbieri F, Luger A, Skalla E, Kountchev J, Widmann G, Plank F.: Myocardial injury in COVID-19: The role of coronary computed tomography angiography (CTA). J Cardiovasc Comput Tomogr. 2020 Jul 17:S1934-5925(20)30391-9. Epub ahead of print.
- Feuchtner G, Langer C, Barbieri F, Beyer C, Dichtl W, Friedrich G, Schgoer W, Widmann G, Plank F.: The effect of omega-3 fatty acids on coronary atherosclerosis quantified by coronary computed tomography angiography. Clin Nutr. 2020 Jul 22:S0261-5614(20)30381-2.
- van Rosendael AR, Narula J, Lin FY, van den Hoogen IJ, Gianni U, Al Hussein Alawamlh O, Dunham PC, Peña JM, Lee SE, Andreini D, Cademartiri F, Chinnaiyan K, Chow BJW, Conte E, Cury RC, Feuchtner G, Hadamitzky M, Kim YJ, Leipsic J, Maffei E, Marques H, de Araújo Gonçalves P, Plank F, Pontone G, Raff GL, Villines TC, Weirich HG, Al’Aref SJ, Baskaran L, Cho I, Danad I, Han D, Heo R, Lee JH, Rivzi A, Stuijfzand WJ, Gransar H, Lu Y, Sung JM, Park HB, Samady H, Stone PH, Virmani R, Budoff MJ, Berman DS, Chang HJ, Bax JJ, Min JK, Shaw LJ.: Association of High-Density Calcified 1K Plaque With Risk of Acute Coronary Syndrome. JAMA Cardiol. 2020 Mar 1;5(3):282-290
Ultrasound
- Morell-Hofert D, Gruber L, Gruber H, Glodny B, Gruber I, Loizides A. Contrast-Enhanced Ultrasound after Endovascular Aortic Repair: Supplement and Potential Substitute for CT in Early- and Long-Term Follow-Up. Ann Vasc Surg. 2024 May;102:9-16. doi: 10.1016/j.avsg.2023.11.040. Epub 2024 Jan 30
- Kosiol J, Keiler A, Loizides A, Gruber H, Henninger B, Bölderl A, Gruber L. Operative versus conservative treatment of acute Achilles tendon ruptures: preliminary results of clinical outcome, kinematic MRI and contrast-enhanced ultrasound. Arch Orthop Trauma Surg. 2023 May;143(5):2455-2465. doi: 10.1007/s00402-022-04457-7.
- Gruber L, Loizides A, Gruber H, Skalla E, Haushammer S, Horlings C, Beer R, Helbok R, Löscher WN. Differentiation of Critical Illness Myopathy and Critical Illness Neuropathy Using Nerve Ultrasonography. J Clin Neurophysiol. 2022 Jan 25. doi: 10.1097/WNP.0000000000000922. Online ahead of print.PMID: 35089907
Interventional Oncology, Stereotaxy & Robotics
- Schullian P, Laimer G, Johnston E, Putzer D, Eberle G, Widmann G, Scharll Y, Bale R.: Reliability of Stereotactic Radiofrequency Ablation (SRFA) for Malignant Liver Tumors: Novice versus Experienced Operators. Biology (Basel). 2023 Jan 22;12(2):175. doi: 10.3390/biology12020175.
- Scharll Y, Letrari S, Laimer G, Schullian P, Bale R.: Puncture accuracy of an optical tracked robotic aiming device-a phantom study. Eur Radiol. 2022 Oct;32(10):6769-6776. doi: 10.1007/s00330-022-08915-z.
- Schullian P, Laimer G, Johnston E, Putzer D, Eberle G, Scharll Y, Widmann G, Kolbitsch C, Bale R.: Technical efficacy and local recurrence after stereotactic radiofrequency ablation of 2653 liver tumors: a 15-year single-center experience with evaluation of prognostic factors. Int J Hyperthermia. 2022;39(1):421-430. doi: 10.1080/02656736.2022.2044522
- Puijk, RS.; Ahmed, M.; Adam, A.; Arai, Y.; Arellano, R.; de Baère, T.; Bale, R.; Bellera, C.; Binkert, CA.; Brace, CL.; Breen, DJ.; Brountzos, E.; Callstrom, MR.; Carrafiello, G.; Chapiro, J.; de Cobelli, F.; Coupé, VMH.; Crocetti, L.; Denys, A.; Dupuy, DE.; Erinjeri, JP.; Filippiadis, D.; Gangi, A.; Gervais, DA.; Gillams, AR.; Greene, T.; Guiu, B.; Helmberger, T.; Iezzi, R.; Kang, TW.; Kelekis, A.; Kim, HS.; Kröncke, T.; Kwan, S.; Lee, MW.; Lee, FT.; Lee, EW.; Liang, P.; Lissenberg-Witte, BI.; Lu, DS.; Madoff, DC.; Mauri, G.; Meloni, MF.; Morgan, R.; Nadolski, G.; Narayanan, G.; Newton, I.; Nikolic, B.; Orsi, F.; Pereira, PL.; Pua, U.; Rhim, H.; Ricke, J.; Rilling, W.; Salem, R.; Scheffer, HJ.; Sofocleous, CT.; Solbiati, LA.; Solomon, SB.; Soulen, MC.; Sze, D.; Uberoi, R.; Vogl, TJ.; Wang, DS.; Wood, BJ.; Goldberg, SN.; Meijerink, MR.: Consensus Guidelines for the Definition of Time-to-Event End Points in Image-guided Tumor Ablation: Results of the SIO and DATECAN Initiative. 2021; 301(3); 533-540. IF: 12,1
- Laimer G, Jaschke N, Schullian P, Putzer D, Eberle G, Solbiati M, Solbiati L, Goldberg SN, Bale R.: Volumetric assessment of the periablational safety margin after thermal ablation of colorectal liver metastases. Eur Radiol. 2021 Sep;31(9):6489-6499. doi: 10.1007/s00330-020-07579-x. Erratum in: Eur Radiol. 2021 Jun 17;: PMID: 33447860
NEURORADIOLOGY
- Mayer-Suess L; Peball, T; Pereverzyev Jr, S; Steiger, R; Galijasevic, M; Kiechl, S; Knoflach, M; Gizewski, E R; Mangesius, S. Cervical artery tortuosity – a reliable semi-automated magnetic resonance-based method. Quantitative Imaging in Medicine and Surgery, 2024. 14(2), 1383-1391.
- Ladenhauf V, Galijasevic M, Regodic M, Helbok R, Rass V, Freyschlag C, Petr O, Deeg J, Gruber L, Mangesius S, Gizewski ER, Grams AE. Aneurysmal Wall Enhancement of Non-Ruptured Intracranial Aneurysmsa after Endovascular Treatment Correlates with Higher Aneurysm Reperfusion Rates, but Only in Large Aneurysms. Diagnostics (Basel). 2024 Jul 16;14(14):1533. doi: 10.3390/diagnostics14141533.
- Thomalla G, Fiehler J, Subtil F, Bonekamp S, Aamodt AH, Fuentes B, Gizewski ER, Hill MD, Krajina A, Pierot L, Simonsen CZ, Zeleňák K, Blauenfeldt RA, Cheng B, Denis A, Deutschmann H, Dorn F, Flottmann F, Gellißen S, Gerber JC, Goyal M, Haring J, Herweh C, Hopf-Jensen S, Hua VT, Jensen M, Kastrup A, Keil CF, Klepanec A, Kurča E, Mikkelsen R, Möhlenbruch M, Müller-Hülsbeck S, Münnich N, Pagano P, Papanagiotou P, Petzold GC, Pham M, Puetz V, Raupach J, Reimann G, Ringleb PA, Schell M, Schlemm E, Schönenberger S, Tennøe B, Ulfert C, Vališ K, Vítková E, Vollherbst DF, Wick W, Bendszus M; TENSION Investigators. Endovascular thrombectomy for acute ischaemic stroke with established large infarct (TENSION): 12-month outcomes of a multicentre, open-label, randomised trial.
Lancet Neurol. 2024 Sep;23(9):883-892. doi: 10.1016/S1474-4422(24)00278-3 - Bendszus M, Fiehler J, Subtil F, Bonekamp S, Aamodt AH, Fuentes B, Gizewski ER, Hill MD, Krajina A, Pierot L, Simonsen CZ, Zeleňák K, Blauenfeldt RA, Cheng B, Denis A, Deutschmann H, Dorn F, Flottmann F, Gellißen S, Gerber JC, Goyal M, Haring J, Herweh C, Hopf-Jensen S, Hua VT, Jensen M, Kastrup A, Keil CF, Klepanec A, Kurča E, Mikkelsen R, Möhlenbruch M, Müller-Hülsbeck S, Münnich N, Pagano P, Papanagiotou P, Petzold GC, Pham M, Puetz V, Raupach J, Reimann G, Ringleb PA, Schell M, Schlemm E, Schönenberger S, Tennøe B, Ulfert C, Vališ K, Vítková E, Vollherbst DF, Wick W, Thomalla G; TENSION Investigators. Endovascular thrombectomy for acute ischaemic stroke with established large infarct: multicentre, open-label, randomised trial. Lancet. 2023 Nov 11;402(10414):1753-1763. doi: 10.1016/S0140-6736(23)02032-9.
- Ladenhauf VK, Galijasevic M, Kerschbaumer J, Freyschlag CF, Nowosielski M, Birkl-Toeglhofer AM, Haybaeck J, Gizewski ER, Mangesius S, Grams AE. Peritumoral ADC Values Correlate with the MGMT Methylation Status in Patients with Glioblastoma. Cancers (Basel). 2023 Feb 22;15(5):1384. doi: 10.3390/cancers15051384
- Gruber N, Galijasevic M, Regodic M, Grams AE, Siedentopf C, Steiger R, et al. A deep learning pipeline for the automated segmentation of posterior limb of internal capsule in preterm neonates. Artif Intell Med. 2022;132:102384.
Selection of Funding
Selection of Competitive Acquired Funding
- FWF grand: “Image Guided Diagnosis and Therapy” (DOC 110-B): Coordinator of PhD projects Prof. Elke R. Gizewski & Prof. Clemens Decristoforo
- DFG: “ACT in Stroke”, Innsbruck-Center Co-PI Prof. Dr. Elke R. Gizewski, cooperation with Anaesthesiology
- EU H2020-SC1-2016-2017, TENSION Study (Efficacy and safety of ThrombEctomy iN Stroke with extended leSION and extended time window: a randomized controlled trial), Prof. Dr. Elke R. Gizewski: Austrian PI)
- VASCage-C: Imaging Biomarkers For Vascular Diseases And Vascular Aging; COMET K1 Zentren 4.Call: 1. FP Partner (FFG), Projektnummer: 6401616; Univ.-Prof. Dr. Elke R. Gizewski
- Subproject Vascage: Post-Stroke Osteopathie; Degenhart Gerald MSc BSc
- KM-induziertes Nierenversagen bei chron. Niereninsuffizienz im Schweinemodell: „CIN- Pig“; MFF Tirol #265; Dr. Anna-Katharina Luger, Assoz.-Prof. PD Dr. Bernhard Glodny
- Basic evaluation of a contrast-free pre-TAVI imaging option: first comparison of a new native MRI protocol with standard-ized contrast-enhanced CT; GHKF Gesellschaft zur Förderung der Herz-Kreislaufforschung in Tirol; Assoz.-Prof. PD Dr. Agnes Mayr
- Long term evolution of infarct scar after reperfused ST-segment elevation myocardial infarction: a 10 year Follow-Up Cardiac Magnetic Resonance Study; ÖKG Österreichische Kardiologische Gesellschaft; Assoz.-Prof. PD Dr. Agnes Mayr
- DISCHARGE Trial : Diagnostic Imaging Strategies: Invasive versus coronary computed tomography angiography for stable chest pain patients with intermediate risk of coronary artery disease: a multicentric randomized pragmatic trial.; 7th Framework Programme (Grant No. 603266) of the European Union.; Ao. Univ.-Prof. Dr. Gudrun Feuchtner
- MedCorpInn – Retrospective Intersectional Corpuslinguistic Analysis of Radiology and Medical Reports of Medical University of Innsbruck; Austrian Academy of Sciences, go!digital 2.0; Mag. Claudia Posch, Karoline Irschara (University of Innsbruck, Institute for Linguistics), PD Dr. Leonhard Gruber, PhD, PD Dr. Stephanie Mangesius, PhD (Universitätsklinik für Radiologie, Medizinische Universität Innsbruck)
- Participation in the FFG COMET programme “Security and safety for shared AI by Deep Model Design”
- Stiftung Propter Homines: Stereotaktische Radiofrequenzablation, PI: Prof. Dr. Reto Bale
- Canadian Sinst of Health Research, Quantitative susceptibility mapping from clinical phase data. PI: Prof. Christoph Birkl (Radiology Innsbruck), Dr. Alex Rauscher (Dept. of Paediatrics, University of British Columbia, Canada).
- FWF Grant “The role of tissue anisotropy in quantitative brain MRI” Grant-DOI 10.55776/I6838 PI: Prof. Christoph Birkl
- TWF: 3D Druck für die Erstellung von individuellen Phantomen für die Dual Energy, PI: PD Dr. Wolfgang Recheis, Dr. Anna Gerstner
- TWF: Quantitative Magnetresonanztomographie bei Patienten mit Carotisstenose vor und nach der Therapie. PI: Prof. Dr. Astrid Grams
Collaborations
- Industry: Siemens Healthcare Erlangen; Interventional Systems, Kitzbühel; Medtronic, Boulder, USA, ASTC Axel Schnaller Technologie Consult, Novartis Institutes for Biomedical research, Biomarker Development- Clinical Imaging
- Leopold Franzens Universität Innsbruck
- Institut für Geologie : Prof. Dr. Michael Strasser & Institut für Mineralogie und Petrographie: Prof. Dr. Peter Tropper; Institut für Archäologien: Prof. Dr. Harald Stadler; Mag. Ulrike Töchterle, Mag. Dr. Martin Auer
- Applied Mathematics: Prof. Dr. Markus Haltmeier & Technische Mathematik: PD Dr. Lukas Neumann; Institut für Mechatronik: Prof. Dr. Daniel Baumgarten; Interactive Graphics and Simulation: Prof. Dr. Matthias Harders
- Klinische Psychologie: Prof. Anna Buchheim, Dr. Karin Labek
- Eidgenössische Technische Hochschule Zürich: Institut für Biomechanik: Univ. Prof. Dr. Ralph Müller; Universitätsklinikum Ulm: Institut für Unfallchirurgische Forschung und Biomechanik: Univ. Dr. Anita Ignatius
- Johannes Keppler Universität: Institut für Physiologie & Pathophysiologie: Univ. Dr. Jakob Völkl
- Software Competence Center Hagenberg, Hagenberg, Austria. Landesmuseum Ferdinandeum: Mag.phil. Wolfgang Sölder
- National Taiwan University: Jyh-Jaan Huang PHD (momentan Forschungsaufenthalt an der LFU Innsbruck)
- Management Centre Innsbruck: Mechatronik- Medizintechnik: Dr. techn. Franz- Josef Falkner
- Rheumatology Department at Vancouver General Hospital (VGH) and Massachusetts General Hospital (MGH): Thomas Jefferson University, PA and Department of Medical Imaging, The University of Arizona Health Network
- Diagnostic and Interventional Radiology, Istituto Ortopedico Galeazzi, Italy
- King Saud University: Prof. Dr. Asma’a al Ekrish Division of Oral and Maxillofacial Radiology, College of Dentistry, Riyadh, Saudi Arabia
- Radon Institute for Computational and Applied Mathematics, Linz, Austria.
- Claudia Lenz, Institute of Forensic Medicine, Department of Biomedical Engineering, University of Basel, Switzerland
- Alexander Rauscher, University of British Columbia, Vancouver, Canada
- Mark E. Ladd. Deutsche Krebsforschungszentrum, Medizinische Physik in der Radiologie, 7T MRT, Heidelberg, Germany
- Martin Bendszus, Prof. Jens Fiehler. Neuroradiologie, Universität Heidelberg & Hamburg, Germany
- Adrian Kastler. Department of Radiology CHU de Grenoble France
- Radiology Department Alexander van Rosendael, Leiden Medical University, Netherlands and Ibrahim Danad, Radboud University Medical Center, Netherlands; and Prof Marc Dewey, Charite Berlin.
- Global Outreach for Radiation Protection Program; Chair, Radiation Safety Committee, Massachusetts General Hospital, Boston, USA.