Anichstraße 35
6020 Innsbruck
Fax: +43 512 504 25857
Email: gert.mayer@i-med.ac.at
Website: https://nephrologie.tirol-kliniken.at/
Research Branch (ÖSTAT Classification)
Keywords
Research Focus
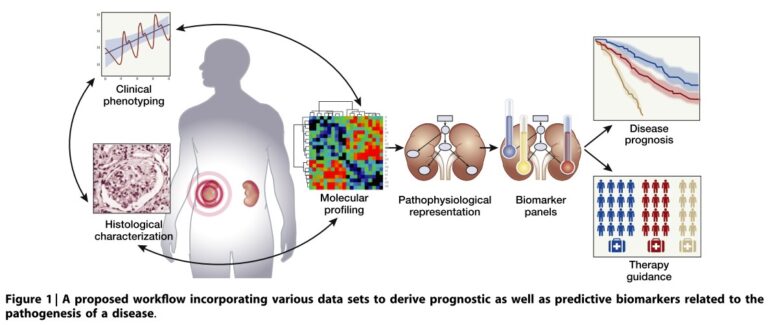
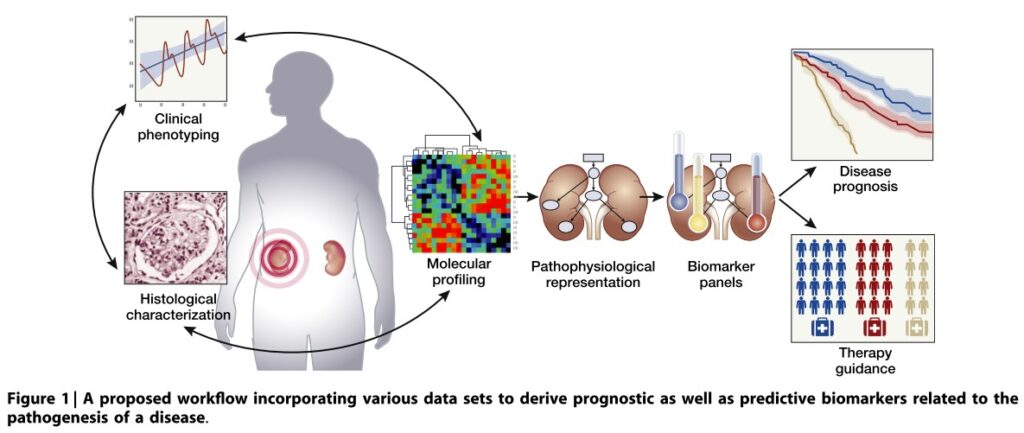
- Precision medicine:The prognosis of patients with renal disease has improved. Yet, cross sectional inter-, and longitudinal intra-individual response to therapy is variable and a better understanding will optimise individual clinical management.
- Epidemiology: The Austrian Dialysis and Transplant Registry collects data from patients with end-stage renal disease. Understanding the epidemiology will provide information on the effectiveness of ESRD and pre-ESRD therapy and will support healthcare planning
General Facts
The Department of Internal Medicine IV (Nephrology and Hypertension) is the primary service provider for Tyrol and the tertiary referral centre for Western Austria and Southern Tyrol for patients with renal diseases and difficult-to-control hypertension (catchment area: ~2 million). We offer an outpatient clinic, an inpatient ward, a dialysis centre, and a routine and a research laboratory. As well as caring for patients with chronic kidney disease and transplant recipients, the outpatient clinic provides special consultations for autoimmune diseases, rare diseases (National Center for Rare Renal Diseases, ERKNET) and the diagnostic work-up/treatment of refractory hypertension (Excellence Center of the European Society of Hypertension). The 20 members of the medical staff perform state-of-the-art sonography and around 100 renal biopsies per year. The Department treats ambulatory haemodialysis dialysis- patients in close collaboration with a local dialysis provider unit and offers a peritoneal dialysis program (CAPD, APD and assisted PD service). The in-house dialysis unit takes care of patients with end-stage as well as acute renal failure and also offers liver replacement therapy, plasmapheresis and immune apheresis for renal, haematological or neurological autoimmune diseases, antibody-mediated transplant rejection and ABO-incompatible renal transplantation. In collaboration with the Department of General and Transplant Surgery, the Innsbruck transplant program offers care for renal transplant living donors and recipients, with 120 – 150 transplants per year.
Research
Precision Medicine in Chronic Kidney Disease (CKD)
DKD: Simone Schmid, Sara Denicolo, Stefani Thöni, Felix Keller, Claudia Zavadil, Clemens Plattner, Sebastian Sallaberger, Susanne Eder, Johannes Leierer, Paul Perco, Markus Pirklbauer, Gert Mayer
CKD: Julia Kerschbaum, Hannes Neuwirt, Michael Rudnicki
Immune-mediated kidney disease: Philipp Gauckler, Andreas Kronbichler
Fluid and electrolyte regulation in endurance sports:
Philipp Gauckler, Andreas Kronbichler
The prognosis of CKD has improved dramatically over the last decades as new treatment options have become available. Following large interventional studies, updated guidelines aim for improving the standard of clinical care in patient cohorts. However, on an individual level, the clinical trajectory and response to therapy of CKD show marked cross-sectional inter-, and longitudinal intra-individual variability. Supported by several European Union grants (Syskid, Beat-DKD, DC-ren, PERSTIGAN, SIGNAL, Kidney Sign), the research focus of the Department is on approaches to the implementation of precision medicine in various CKD settings.
A. Diabetic kidney disease (DKD):
It has become obvious that renal impairment in patients with diabetes mellitus is a complex phenotype with heterogeneous prognosis and response to therapy. Computational systems biology using multi-omics data and advanced disease-modelling techniques (such as the application of dynamic systems theory-tools) are employed to offer better understanding and description of the clinical course, pathophysiology and response to therapy of DKD on an individual clinical and molecular level. The major aims are:
(i) To decipher intrinsic kidney-protective mechanisms and identify novel therapeutic targets,
(ii) To identify and apply prognostic and predictive biomarkers/biomarker panels in clinic,
(iii) To investigate drug mechanisms of action in relation to disease pathophysiology.
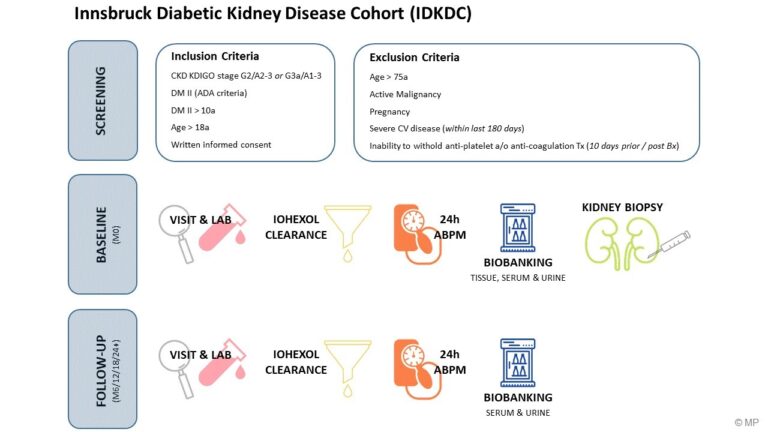
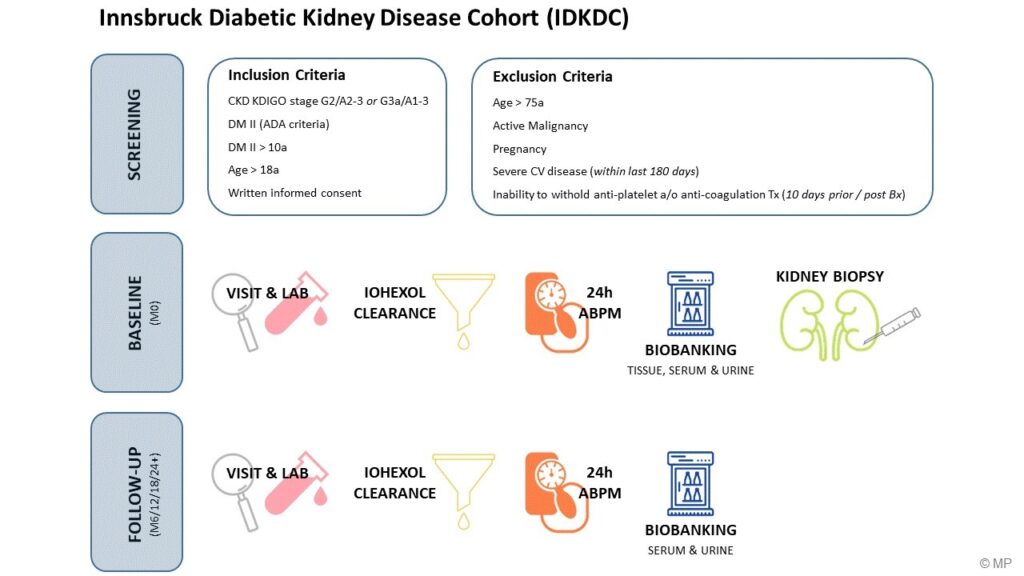
In line with these efforts, we initiated the Innsbruck Diabetic Kidney Disease Cohort. Patients with early renal dysfunction undergo a kidney biopsy to assess the individual histopathological phenotype. Extensive bio-banking over a follow-up period of five years will support future projects. This complements the repository of the prospective observational international cohort study PROVALID recruited 4,000 patients with type 2 diabetes mellitus, with follow-ups of at least four years.
b. IgA Nephropathy:
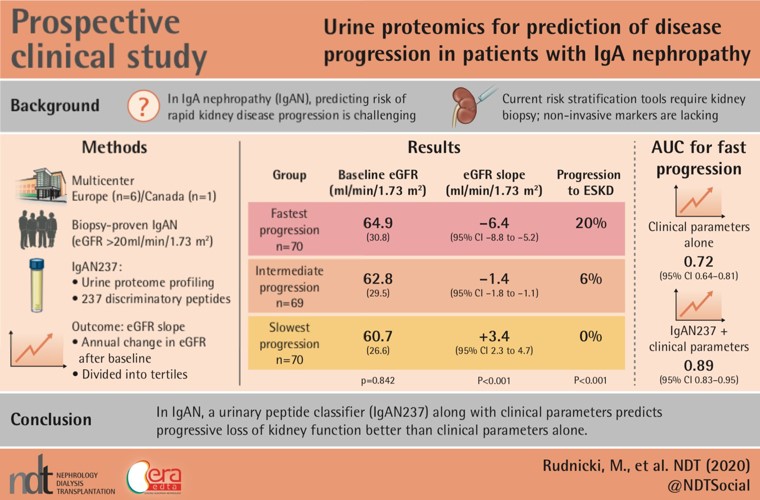
Kidney function decline in IgA nephropathy (IgAN) can be significant and is not predictable using the available clinical and histological tools. The EU/FWF-funded program PERSTIGAN identified a urinary biomarker-based classifier (IgAN237), which showed significant benefit for the prediction of disease progression compared with the clinical parameters (age, gender, proteinuria, eGFR, mean arterial pressure). This proteomic panel is available as an online risk calculator (perstigan.eu), and is undergoing further evaluation of its potential to guide treatment decisions in a prospective clinical trial.
c. Immune-mediated kidney disease:
The team is among the world’s leading experts in the field (as revealed by expertscape). State-of-the-art treatment includes novel and emerging therapies and the conduct of several clinical trials in these rare diseases.
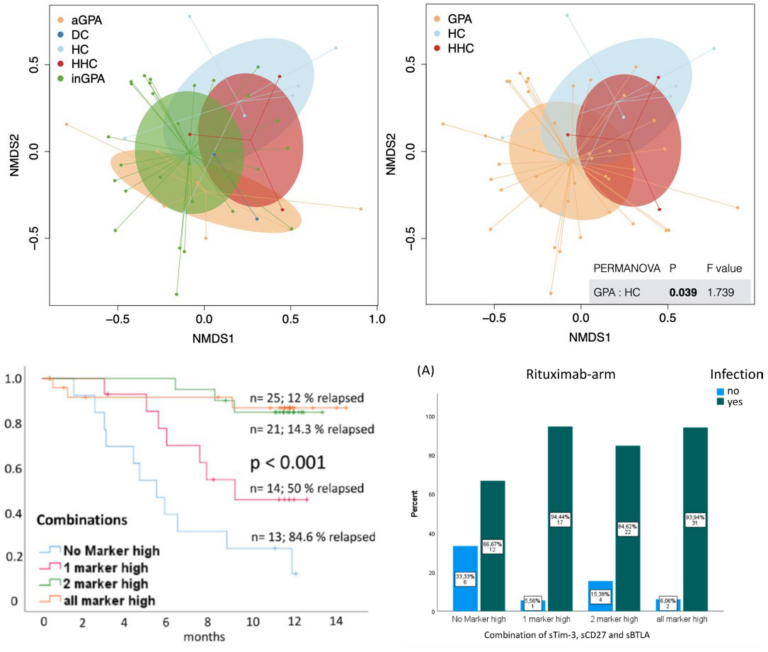
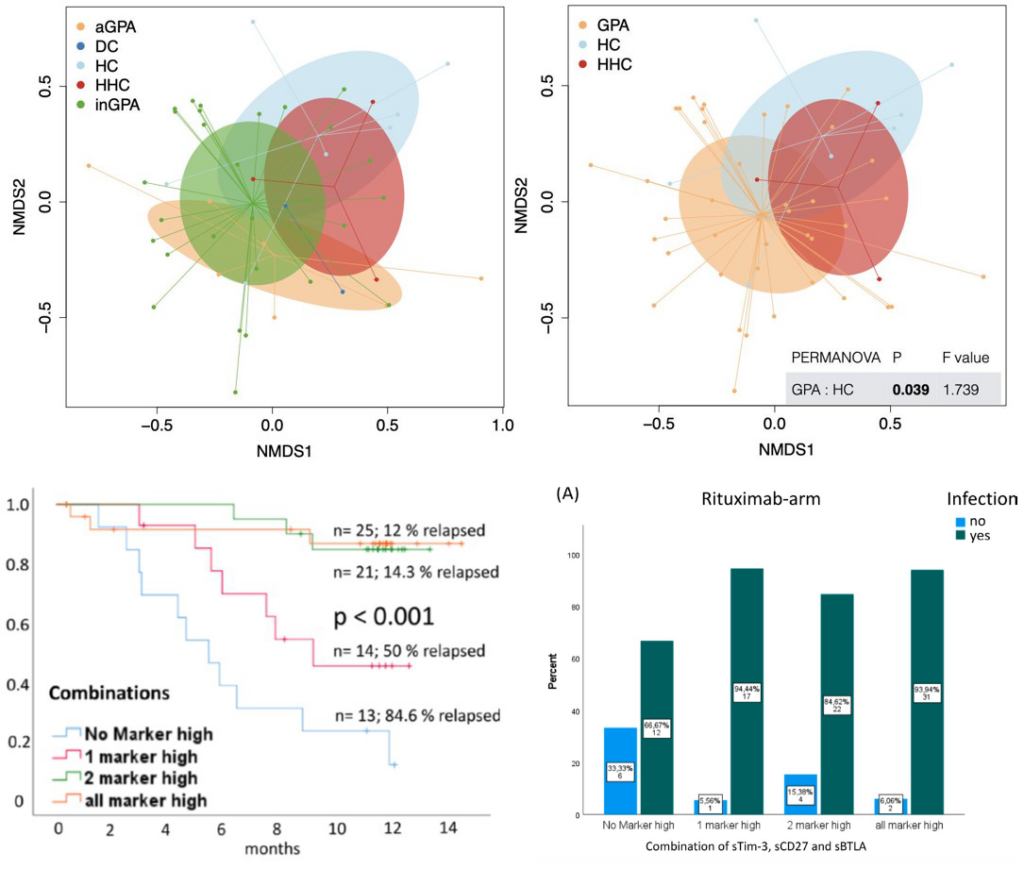
Several high-impact papers have been published by the team over the past years, enabling precision medicine by monitoring the “immunocompetence” of the host, tailoring the immunosuppression based on an individual’s need. We have recently identified that a higher expression of soluble immune checkpoints at baseline is indicating a lower risk of disease relapse in individuals with PR3-ANCA vasculitis; however, these patients have a higher risk of infections. The concept of “immunocompetence” will be further investigated by assessing the impact of torque teno virus as a risk predictor of infections / relapse in autoimmune disease, the impact of “exhausted markers” of T- and B-cell activation, outcomes research and staining of kidney biopsies. The team has ongoing collaborations with groups from South and North America, Asia and across Europe. A registry on rituximab use in nephrotic syndrome (RITERM) has collected data on 448 patients and will likely generate helpful information related to the future use of this drug in this indication.
Other international projects are focusing on treatment response variability in ANCA-associated vasculitides and nephrotic diseases.
d. Haemodialysis:
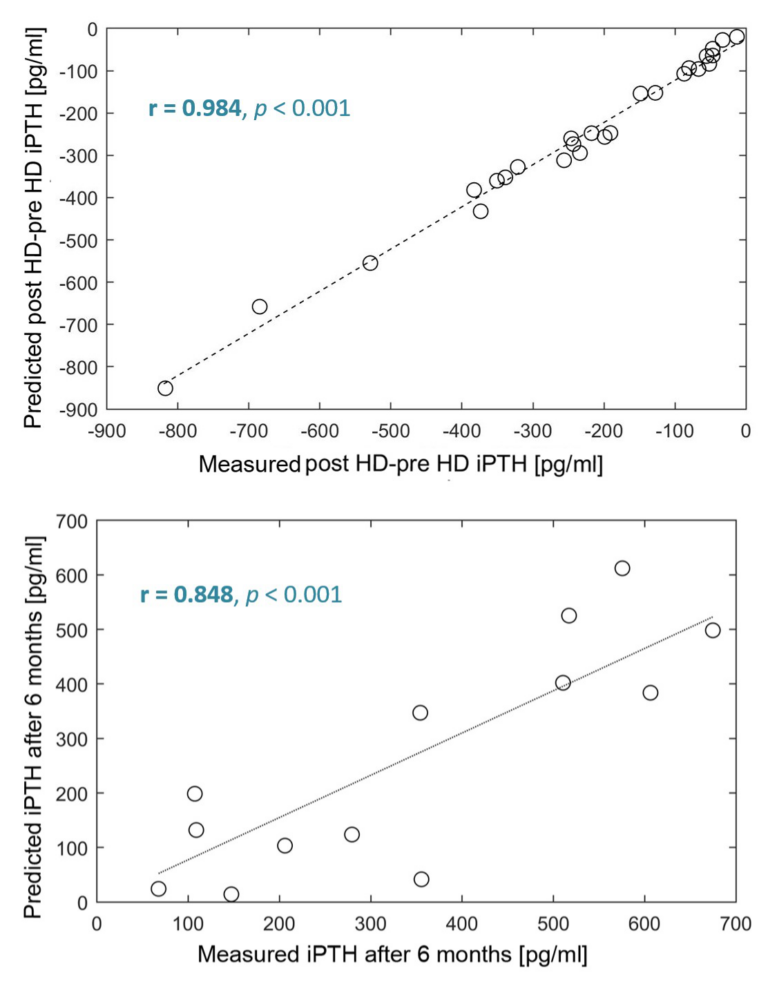
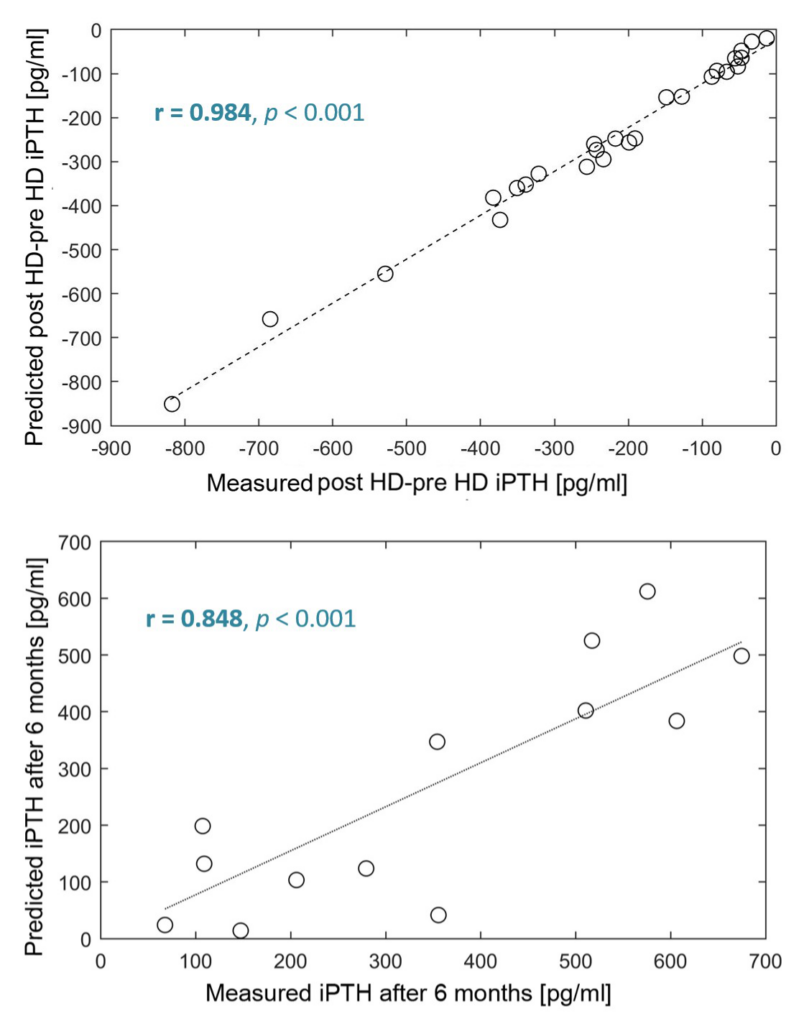
Patients on renal replacement therapy suffer from excessive cardiovascular morbidity and mortality. The assessment of individual calcium kinetics during dialysis serves as an example for the study of individual heterogeneity in response to fixed, guideline-recommended dialysis prescription in a population. CKD-associated mineral bone disorders, including secondary hyperparathyroidism, are causally related to increased cardiovascular morbidity and mortality among haemodialysis patients. In this regard, we validated the individualisation of a physiology-based mathematical model of parathyroid gland biology by predicting the patients’ short-term peridialytic iPTH changes in response to diffusive intradialytic Ca loading. We then used this mathematical model to predict the level of iPTH at 6-months using only readily available clinical data, such as iCa and phosphate measurements, iPTH history, dialysis vintage and information about vitamin D therapy (Fig. 5 and 6).
e. Renal transplantation:
Individual adaption of immunosuppressive therapy is crucial for long-term transplant as well as recipient survival. Research is focusing on immune surveillance using torque teno virus-guided therapy and optimised selection of drug combinations. In collaboration with the Department of General, Visceral and Transplant Surgery, work on an ex vivo organ perfusion system is ongoing.
f. Fluid and electrolyte regulation in endurance sports:
Ultra-endurance cyclists expose themselves to extreme physical challenges. Recently, a high rate of ”swelling symptoms“ during or after an ultra-cycling race was reported in a large cohort of athletes, yet little is known about underlying mechanisms. In this research project, we aim to study the occurrence of peripheral oedema in ultra-cyclists and elucidate underlying (patho)-physiological processes.
The Austrian Dialysis and Transplant Registry (ÖDTR)
Daniela Kaiser-Feistmantl, Lukas Buchwinkler, Julia Kerschbaum, Gert Mayer
Since the 1960s, the Austrian Dialysis and Transplant Registry has collected individual data on all patients with end-stage renal disease who require dialysis or kidney transplantation. Since its move to Innsbruck in 2018, the registry has undergone transformation into web-based data repository, following rules set out in GDPR. The ÖDTR supports national healthcare authorities in the planning of regional dialysis-facility resource allocation. In addition, it provides various quality-control programs of the Austrian Society of Nephrology. Because of the high quality and completeness of the data collected, the registry is also an outstanding source for academic research. In addition to internal projects, the ÖDTR collaborates with national and international researchers and organisations (such as the European Renal Association) under the guidance of an external advisory board.
Pictures
Selected Publications
Odler B, Riedl R, Gauckler P, Shin JI, Leierer J, Merkel PA, St Clair W, Fervenza F, Geetha D, Monach P, Jayne D, Smith RM, Rosenkranz A, Specks U, Stone JH, Kronbichler A; RAVE−ITN Research Group: Risk factors for serious infections in ANCA-associated vasculitis. Annals of the rheumatic diseases 2023;ard-2022-223401
Perco P, Mayer G: The kidney-more than the sum of its cellular parts. Kidney Int 2022; 102:1217-1219
Denicolò S, Laydevant S, Fink J, Geiger C, Pizzini A, Sarcletti M, Zschocke J, Bellmann-Weiler R, Weiss G, Tancevski I: Sarcoid-like lesions obfuscating the diagnosis of disseminated Mycobacterium genavense infection in a patient with IL-12Rβ1-associated immunodeficiency. BMC Infect Dis. 2022; 22(1):770. doi: 10.1186/s12879-022-07644-4
Thöni S, Keller F, Denicolò S, Buchwinkler L, Mayer G: Biological variation and reference change value of the estimated glomerular filtration rate in humans: A systematic review and meta-analysis. Front Med (Lausanne). 2022; 9:1009358. doi: 10.3389/fmed.2022.1009358
Thöni S, Keller F, Denicoló S, Eder S, Buchwinkler L, Rosivall L, Wiecek A, Mark P.B, Rossing P, Heerspink H.J.L., Mayer G: International variability of renal and cardiovascular outcomes and mortality in patients with type 2 diabetes mellitus in Europe. Kidney Blood Press Res. Accepted 2022-11-23. In press. doi: 10.1159/000528438
Sallaberger S, Buchwinkler L, Eder S, Schneeberger S, Mayer G, Pirklbauer M: Population characteristics and clinical outcome from the renal transplant outcome prediction validation study (TOPVAS) J Clin Med 2022; 11:7421. doi: 10.1038/s41598-022-11198-5
Stigler J, Buchwinkler L, Solagna CA, Rudnicki M, Pirklbauer M, Mayer G, Kerschbaum J: Humoral immune response to a timely booster mRNA vaccination in non-responders to a standard vaccination schedule against COVID-19 in kidney transplant recipients. J Clin Med 2022; 11:6439. doi: 103390/jcm11216439
Smeijer JD, Koomen JV, Kohan DE, McMurray JJV, Bakris GL, Correa-Rotter R, Hou FF, Kitzman DW, Makino H, Mayer G, Nowicki M, Perkovic V, Rossing P, Tobe S, Parving HH, de Zeeuw D, Heerspink HJL: Organic anion transporter gene variants associated with plasma exposure and long-term response to atrasentan in patients with diabetic kidney disease. Clin Pharmacol Ther. 2022. doi: 10.1002/cpt.2721
Agarwal R, Burton J, Gallieni M, Kalantar-Zadeh K, Mayer G, Pollock C, Szeptietowski JC: Alleviating symptoms in patients undergoing long-term hemodialysis: a focus on chronic kidney disease associated pruritus. Clin Kidney J 2022; 16:30-40
Huber C, Krauss M, Reinstadler V, Denicolo S, Mayer G, Schulze T, Brack W, Oberacher H: In silico deconjugation of glucuronide conjugates enhances tandem mass spectra library annotation of human samples. Anal Bioanal Chem 2022; 414:2629-2640
Stigler J, Buchwinkler L, Solagna CA, Rudnicki M, Pirklbauer M, Mayer G, Kerschbaum J: Humoral immune response to a timely booster mRNA vaccination in non-responders to a standard vaccination schedule against COVID-19 in kidney transplant recipients. Clin Med 2022. doi 103390/jcm11216439
Thöni S, Keller F, Denicolo S, Buchwinkler L, Mayer G: Biological variation and reference change value of estimated glomerular filtration rate in humans: a systemic review and metaanalysis. Front Med 2022. doi:10.3389/fmed.2022.10093358
Säemann M, Cejka D, Schmaldienst S, Rosenkranz AR, Mayer G: Value of SGLT-2 inhibitors in the treatment of chronic kidney disease: Clinical and practical implications. Wien Klin Wochenschr 2022. doi: 10.1007/s00508-022-02096-x
Denicolo S, Nair V, Leierer J, Rudnicki M, Kretzler M, Mayer G, Ju W, Perco P: Assessment of Fibrinogen-like 2 (FGL2) in human chronic kidney disease through transcriptomic data analysis. Biomolecules 2022. doi: 10.3390/biom13010089
Ranches G, Zeidler M, Kessler R, Hoelzl M, Hess MW, Vosper J, Perco P, Schramek H, Kummer KK, Kress M, Krogsdam A, Rudnicki M, Mayer G, Huettenhofer A: Exosomal mitochondrial tRNAs and miRNAs as potential predictors of inflammation in renal proximal tubular epithelial cells. Mol Ther Nucleic Acids. 2022; 4;28:794-813. doi: 10.1016/j.omtn.2022.04.035
Denicolo S, Vogi V, Keller F, Thöni S, Eder S, Heerspink HJL, Rosivall L, Wiecek A, Mark PB, Perco P, Leierer J, Kronbichler A, Steger M, Schwendinger S, Zschocke J, Mayer G, Jukic E: Clonal hematopoiesis of indeterminate potential and diabetic kidney disease: a nested case control study. Kidney Int Rep. 2022. doi:10.1016/j.ekir.2022.01.1064
Huber C, Krauss M, Reinstadler V, Denicolò S, Mayer G, Schulze T, Brack W, Oberacher H: In silico deconjugation of glucuronide conjugates enhances tandem mass spectra library annotation of human samples. Anal Bioanal Chem. 2022. doi: 10.1007/s00216-022-03899-7
Kainz A, Kammer M, Reindl-Schwaighofer R, Strohmaier S, Petr V, Viklicky O, Abramowicz D, Naik M, Mayer G, Oberbauer R: Waiting time for second kidney transplantation and mortality. Clin J Am Soc Nephrol. 2022; 17:90-97. doi: 10.2215/CJN.07620621
Salas A, Kant S, Floyd L, Kratky V, Brix SR, Prendecki M, Schönermarck U, Scott J, Saha M, Gauckler P, Li T, Sharma PD, Ayoub I, Morris AD, Dhaygude AP, Hruskova Z, Tesar V, McAdoo SP, Little MA, Derebail VK, Poulton CJ, Seo P, Kronbichler A, Geetha D: ANCA Vasculitis Induction Management During the COVID-19 Pandemic. Kidney Int Rep. 2021;6(11):2903-2907
Bakker E, Mol PGM, Nabais J, Vetter T, Kretzler M, Nolan JJ, Mayer G, Sundgren AK, Heerspink HJL, Schiel A, de Vries ST, Gomez MF, Schulze F, de Zeeuw D, Pena MJ: Perspectives on a way forward to implementation of precision medicine in patients with diabetic kidney disease; Results of a stakeholder consensus-building meeting. Front Pharmacol. 2021; 12:662642. doi: 10.3389/fphar.2021.662642
Pirklbauer M, Bushinsky DA, Kotanko P, Schappacher-Tilp G: Personalized prediction of short- and long-term PTH changes in maintenance hemodialysis patients. Front Med. 2021; 8:704970
Buchwinkler L, Solagna CA, Messner J, Pirklbauer M, Rudnicki M, Mayer G, Kerschbaum J: Antibody response to mRNA vaccines against SARS-CoV-2 with chronic kidney disease, hemodialysis, and after kidney transplantation. J Clin Med. 2021; 11:148. doi: 10.3390/jcm11010148
Gregorich M, Heinzel A, Kammer M, Meiselbach H, Böger C, Eckardt KU, Mayer G, Heinze G, Oberbauer R: A prediction model for the decline in renal function in people with type 2 diabetes mellitus: study protocol. Diagn Progn Res. 2021; 5:19. doi: 10.1186/s41512-021-00107-5.PMID:34789343
Thöni S, Mayer G: Urinary Dickkopf-3 and kidney injury in patients with chronic pulmonary disease. Kidney Int 2021; 100:983-985. doi: 10.1016/j.kint.2021.08.012
Pirklbauer M, Sallaberger S, Staudinger P, Corazza U, Leierer J, Mayer G, Schramek H: Empagliflozin inhibits IL-1β-mediated inflammatory response in human proximal tubular cells. Int J Mol Sci. 2021; 22:5089. doi: 10.3390/ijms22105089
Garam N, Mayer G et al. FHR-5 serum levels and CFHR5 genetic variations in patients with immune complex-mediated membranoproliferative glomerulonephritis and C3-glomerulopathy. Front Immunol. 2021; 12:720183. doi: 10.3389/fimmu.2021.720183
Gauckler P, Bettac EL, Nairz M, Duftner C, Luger AK, Stein M, Wanner D, Böckle BC, Tiefenthaler M, Schratzberger P, Neuwirt H, Harasser L, Mayer G, Kronbichler A: What comes after the lockdown? Clustering of ANCA-associated vasculitis: single-centre observation of a spatiotemporal pattern. Ann Rheum Dis. 2021; 80:669-671. doi: 10.1136/annrheumdis-2020-219212
Effenberger M, Kronbichler A, Bettac E, Grabherr F, Grander C, Adolph TE, Mayer G, Zoller H, Perco P, Tilg H: Using infodemiology metrics to assess public interest in liver transplantation: Google trends analysis. J Med Internet Res. 2021; 23: e21656. doi: 10.2196/21656
Prischl FC, Rossing P, Bakris G, Mayer G, Wanner C: Major adverse renal events (MARE): a proposal to unify renal endpoints. Nephrol Dial Transplant. 2021; 36:491-497. doi: 10.1093/ndt/gfz212
Leierer J, Perco P, Hofer B, Eder S, Dzien A, Kerschbaum J, Rudnicki M, Mayer G: Coregulation analysis of mechanistic biomarkers in autosomal dominant polycystic kidney disease. Int J Mol Sci. 2021; 22:6885. doi: 10.3390/ijms22136885
Vlahou A, Mayer G et al. Data sharing under the general data protection regulation: time to harmonize law and research ethics? Hypertension. 2021; 77:1029-1035. doi: 10.1161/HYPERTENSIONAHA.120.16340
Denicolò S, Perco P, Thöni S, Mayer G: Non adherence to antidiabetic and cardiovascular drugs in type 2 diabetes mellitus and its association with renal and cardiovascular outcomes: A narrative review. J Diabetes Complications. 2021; 35:107931. doi: 10.1016/j.jdiacomp.2021.107931
Mayer G: Precision medicine in nephrology. Nephrol Dial Transplant. 2021; 36(Suppl 2):1-2. doi: 10.1093/ndt/gfaa366
Beer AGE, Laille E, Neuwirt H, Mayer G, Stauder R: Azacitidine is removed effectively by hemodialysis. Leuk Lymphoma. 2021; 62:743-745. doi: 10.1080/10428194.2020
Gauckler P, Shin JI, Alberici F, Audard V, Bruchfeld A, Busch M, Cheung CK, Crnogorac M, Delbarba E, Eller K, Faguer S, Galesic K, Griffin S, van den Hoogen MWF, Hrušková Z, Jeyabalan A, Karras A, King C, Kohli HS, Mayer G, Maas R, Muto M, Moiseev S, Odler B, Pepper RJ, Quintana LF, Radhakrishnan J, Ramachandran R, Salama AD, Schönermarck U, Segelmark M, Smith L, Tesař V, Wetzels J, Willcocks L, Windpessl M, Zand L, Zonozi R, Kronbichler A; RITERM study group.: Rituximab in Membranous Nephropathy. Kidney Int Rep. 2021;6(4):881-893
Gauckler P; Kesenheimer JS; Kronbichler A; Kolbinger FR: Edema-like symptoms are common in ultra-distance cyclists and driven by overdrinking, use of analgesics and female sex – a study of 919 athletes. Journal of the international society of sports nutrition 2021;18(1):73
Pirklbauer M, Bernd M, Fuchs L, Staudinger P, Corazza U, Leierer J, Mayer G, Schramek H: Empagliflozin inhibits basal and IL-1β-mediated MCP-1/CCL2 and endothelin-1 expression in human proximal tubular cells. Int J Mol Sci. 2020; 21:8189. doi: 10.3390/ijms21218189
Kerschbaum J, Rudnicki M, Dzien A, Dzien-Bischinger C, Winner H, Heerspink HL, Rosivall L, Wiecek A, Mark PB, Eder S, Denicolò S, Mayer G: Intra-individual variability of eGFR trajectories in early diabetic kidney disease and lack of performance of prognostic biomarkers. Sci Rep. 2020; 10:19743. doi: 10.1038/s41598-020-76773-0
Ganz T, Aronoff GR, Gaillard CAJM, Goodnough LT, Macdougall IC, Mayer G, Porto G, Winkelmayer WC, Wish JB: Iron administration, infection, and anemia management in CKD: untangling the effects of intravenous iron therapy on immunity and infection risk. Kidney Med. 2020; 2:341-353. doi: 10.1016/j.xkme.2020.01.006
Kerschbaum J, Bitter S, Weitlaner M, Kienzl-Wagner K, Neuwirt H, Bösmüller C, Mayer G, Schneeberger S, Rudnicki M: Arterial hypertension as a risk factor for reduced glomerular filtration rate after living kidney donation. J Clin Med. 2020; 9:338. doi: 10.3390/jcm9020338
Gauckler P, Shin JI, Alberici F, Audard V, Bruchfeld A, Busch M, Cheung CK, Crnogorac M, Delbarba E, Eller K, Faguer S, Galesic K, Griffin S, Hrušková Z, Jeyabalan A, Karras A, King C, Kohli HS, Maas R, Mayer G, Moiseev S, Muto M, Odler B, Pepper RJ, Quintana LF, Radhakrishnan J, Ramachandran R, Salama AD, Segelmark M, Tesař V, Wetzels J, Willcocks L, Windpessl M, Zand L, Zonozi R, Kronbichler A; RITERM study group.: Rituximab in adult minimal change disease and focal segmental glomerulosclerosis – What is known and what is still unknown? Autoimmun Rev. 2020; 19:102671. doi: 10.1016/j.autrev.2020.102671
Gauckler P, Leierer J, Kocher F, Feistritzer C, Willenbacher W, Gunsilius E, Wolf D, Neuwirt H, Mayer G, Kronbichler A: Lessons learned from immunoadsorption for hyperviscosity in IgM multiple myeloma-A case report. J Clin Apher. 2020; 35:227-230. doi: 10.1002/jca.21775
Kronbichler A, Shin JI, Lee KH, Nakagomi D, Quintana LF, Busch M, Craven A, Luqmani RA, Merkel PA, Mayer G, Jayne DRW, Watts RA: Clinical associations of renal involvement in ANCA-associated vasculitis. Autoimmun Rev. 2020; 19:102495. doi: 10.1016/j.autrev.2020.102495
Kronbichler A, Effenberger M, Shin JI, Koppelstätter C, Denicolò S, Rudnicki M, Neuwirt H, Soler MJ, Stevens K, Bruchfeld A, Tilg H, Mayer G, Perco P: Is there decreasing public interest in renal transplantation? A Google TrendsTM Analysis. J Clin Med. 2020; 9:1048. doi: 10.3390/jcm9041048
Watschinger B, Watschinger C, Reindl-Schwaighofer R, Meyer EL, Deak AT, Hammer T, Eigner M, Sprenger-Mähr H, Schneeberger S, Cejka D, Mayer G, Oberbauer R, Rosenkranz AR, Kerschbaum J: Impact of timely public health measures on kidney transplantation in Austria during the SARS-CoV-2 outbreak-a nationwide analysis. J Clin Med. 2020; 9:3465. doi: 10.3390/jcm9113465
Pirklbauer M, Fuchs L, Heiss R, Ratschiller T, Mayer G: Intradialytic calcium kinetics and cardiovascular disease in chronic hemodialysis patients. Blood Purif. 2020; 49:723-732. doi: 10.1159/000508060
Effenberger M, Kronbichler A, Shin JI, Mayer G, Tilg H, Perco P: Association of the COVID-19 pandemic with Internet Search Volumes: A Google TrendsTM Analysis. Int J Infect Dis. 2020; 95:192-197. doi: 10.1016/j.ijid.2020.04.033
Gasteiger S, Berchtold V, Bösmüller C, Dostal L, Ulmer H, Bogensperger C, Resch T, Rudnicki M, Neuwirt H, Oberhuber R, Cardini B, Scheidl S, Mayer G, Öfner D, Weissenbacher A, Schneeberger S: A retrospective propensity score matched analysis reveals superiority of hypothermic machine perfusion over static cold storage in deceased donor kidney transplantation. J Clin Med. 2020; 9:2311. doi: 10.3390/jcm9072311
Jager KJ, Kramer A, Chesnaye NC, Couchoud C, Sánchez-Álvarez JE, Garneata L, Collart F, Hemmelder MH, Ambühl P, Kerschbaum J, Legeai C, Del Pino Y Pino MD, Mircescu G, Mazzoleni L, Hoekstra T, Winzeler R, Mayer G, Stel VS, Wanner C, Zoccali C, Massy ZA: Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int 2020; 98:1540-1548. doi: 10.1016/j.kint.2020.09.006
Rudnicki M, Siwy J, Wendt R, Lipphardt L, Koziolek MJ, Maixnerova D, Peters B, Kerschbaum J, Leierer J, Neprasova M, Banasik M, Sanz AB, Perez-Gomez MV, Ortiz A, Stegmayr B, Tesar V, Mischak H, Beige J, Reich HN on behalf of the PERSTIGAN working group: Urine proteomics for prediction of disease progression in patients with IgA nephropathy. Nephrology Dialysis & Transplantation. 2020 in press
Kronbichler A, Gauckler P, Windpessl M, Shin JI, Jha V, Rovin BH, Oberbauer R: COVID-19: implications for immunosuppression in kidney disease and transplantation. Nature Reviews in nephrology. 2020; 16, 365-367
Pippias M, Jager KJ, Åsberg A, Berger SP, Finne P, Heaf JG, Kerschbaum J, Lempinen M, Magaz Á, Massy ZA, Stel VS: Young deceased donor kidneys show a survival benefit over older donor kidneys in transplant recipients aged 20-50 years: a study by the ERA-EDTA Registry. Nephrology Dialysis & Transplantation 2020; 35; 534-543
Heerspink HJL, Perco P, Mulder S, Leierer J, Hansen MK, Heinzel A, Mayer G: Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia. 2019; 62:1154-1166. doi: 10.1007/s00125-019-4859-4
Mayer GJ, Wanner C, Weir MR, Inzucchi SE, Koitka-Weber A, Hantel S, von Eynatten M, Zinman B, Cherney DZI: Analysis from the EMPA-REG OUTCOME trial indicates empagliflozin may assist in preventing the progression of chronic kidney disease in patients with type 2 diabetes irrespective of medications that alter intrarenal hemodynamics. Kidney Int 2019; 96:489-504. doi: 10.1016/j.kint.2019.02.033
Sourij H, Edlinger R, Prischl FC, Auinger M, Kaser S, Horn S, Paulweber B, Kautzky-Willer A, Säemann M, Prager R, Clodi M, Schernthaner G, Mayer G, Oberbauer R, Rosenkranz AR: Diabetic kidney disease (Update 2019): Position paper of the Austrian Diabetes Association and the Austrian Society for Nephrology. Wien Klin Wochenschr. 2019; 131(Suppl 1):151-163. doi: 10.1007/s00508-018-1425-x
Neuwirt H, Burtscher A, Cherney D, Mayer G, Ebenbichler C: Tubuloglomerular feedback in renal glucosuria: mimicking ong-term SGLT-2 inhibitor therapy. Kidney Med. 2019; 2:76-79. doi: 10.1016/j.xkme.2019.09.006
Weber T, Mayer G et al: Austrian Consensus on High Blood Pressure 2019. Wien Klin Wochenschr. 2019; 131(Suppl 6):489-590. doi: 10.1007/s00508-019-01565-0
Kronbichler A, Gauckler P, Lee KH, Shin JI, Malvezzi P, Mayer G: Immunoadsorption in nephrotic syndrome: Where are we now and where are we going from here? Atheroscler Suppl. 2019; 40:55-60. doi: 10.1016/j.atherosclerosissup.2019.08.027
Garam N, Mayer G et al: C4 nephritic factor in patients with immune-complex-mediated membranoproliferative glomerulonephritis and C3-glomerulopathy. Orphanet J Rare Dis. 2019; 14:247. doi: 10.1186/s13023-019-1237-8
Perco P, Ju W, Kerschbaum J, Leierer J, Menon R, Zhu C, Kretzler M, Mayer G, Rudnicki M: Identification of dicarbonyl and L-xylulose reductase as a therapeutic target in human chronic kidney disease. JCI Insight. 2019; 4: e128120. doi: 10.1172/jci.insight.128120
Kammer M, Heinzel A, Willency JA, Duffin KL, Mayer G, Simons K, Gerl MJ, Klose C, Heinze G, Reindl-Schwaighofer R, Hu K, Perco P, Eder S, Rosivall L, Mark PB, Ju W, Kretzler M, McCarthy MI, Heerspink HL, Wiecek A, Gomez MF, Oberbauer R: Integrative analysis of prognostic biomarkers derived from multiomics panels helps discrimination of chronic kidney disease trajectories in people with type 2 diabetes. Kidney Int 2019; 96:1381-1388. doi: 10.1016/j.kint.2019.07.025
Weissenbacher A, Oberhuber R, Hermann M, Soleiman A, Ulmer H, Mayer G, Margreiter C, Maglione M, Bösmüller C, Messner F, Resch T, Cardini B, Troppmair J, Margreiter R, Öfner D, Schneeberger S: Live confocal tissue assessment with SYTO16/PI and WGA staining visualizes acute organ damage and predicts delayed graft function in kidney transplantation. Ann Surg. 2019; 270:915-922. doi: 10.1097/SLA.0000000000003511
Garam N, Mayer G et al: Validation of distinct pathogenic patterns in a cohort of membranoproliferative glomerulonephritis patients by cluster analysis. Clin Kidney J. 2019; 13:225-234. doi: 10.1093/ckj/sfz073
Wagner J, Harrison EM, Martinez Del Pero M, Blane B, Mayer G, Leierer J, Gopaluni S, Holmes MA, Parkhill J, Peacock SJ, Jayne DRW, Kronbichler A: The composition and functional protein subsystems of the human nasal microbiome in granulomatosis with polyangiitis: a pilot study. Microbiome. 2019; 7:137. doi: 10.1186/s40168-019-0753-z
Koppelstaetter C, Leierer J, Rudnicki M, Kerschbaum J, Kronbichler A, Melk A, Mayer G, Perco P: Computational drug screening identifies compounds targeting renal age-associated molecular profiles. Comput Struct Biotechnol J. 2019; 17:843-853. doi: 10.1016/j.csbj.2019.06.019
Jordan H, Mayer G et al: Management of supine hypertension in patients with neurogenic orthostatic hypotension: scientific statement of the American Autonomic Society, European Federation of Autonomic Societies, and the European Society of Hypertension. J Hypertens. 2019; 37:1541-1546. doi: 10.1097/HJH.0000000000002078
Neuwirt H, Leitner-Lechner I, Kerschbaum J, Ertl M, Pöggsteiner F, Pölt N, Mätzler J, Sprenger-Mähr H, Rudnicki M, Schratzberger P, Eder IE, Mayer G: Efficacy and safety of Belatacept treatment in renal allograft recipients at high cardiovascular risk – a single center experience. J Clin Med. 2019; 8:1164. doi: 10.3390/jcm8081164
Kronbichler A, Leierer J, Shin JI, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, Kallenberg CGM, St Clair EW, Brunetta P, Fervenza FC, Geetha D, Keogh KA, Monach PA, Ytterberg SR, Mayer G, Specks U, Stone JH, RAVE−ITN Research Group: Association of pulmonary hemorrhage, positive proteinase 3, and urinary red blood cell casts with venous thromboembolism in antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis&Rheumatology. 2019; 71:1888-1893. doi: 10.1002/art.41017
Eder S, Leierer J, Kerschbaum J, Rosivall L, Wiecek A, de Zeeuw D, Mark PB, Heinze G, Rossing P, Heerspink HL, Mayer G: Guidelines and clinical practice at the primary level of healthcare in patients with type 2 diabetes mellitus with and without kidney disease in five European countries. Diab Vasc Dis Res. 2019; 16:47-56. doi: 10.1177/1479164118795559
Pirklbauer M, Schupart R, Fuchs L, Staudinger P, Corazza U, Sallaberger S, Leierer J, Mayer G, Schramek H: Unravelling reno-protective effects of SGLT2 inhibition in human proximal tubular cells. Am J Physiol Renal Physiol. 2019; 316: F449-F462. doi: 10.1152/ajprenal.00431.2018
Perco P, Ju W, Kerschbaum J, Leierer J, Menon R, Zhu C, Kretzler M, Mayer G, Rudnicki M; Nephrotic Syndrome Study Network (NEPTUNE): Identification of dicarbonyl and L-xylulose reductase as a therapeutic target in human chronic kidney disease. Journal of clinical investigation inside. 2019; 4: e128120.
Gauckler P, Shin JI, Mayer G, Kronbichler A: Eosinophilia and kidney disease: more than just an incidental finding? J Clin Med. 2018; 7:529. doi: 10.3390/jcm7120529
de Vries JK, Levin A, Loud F, Adler A, Mayer G, Pena MJ: Implementing personalized medicine in diabetic kidney disease: Stakeholders’ perspectives. Diabetes Obes Metab. 2018; 20 (Suppl3):24-29. doi: 10.1111/dom.13412
Perco P, Pena M, Heerspink HJL, Mayer G: Multimarker panels in diabetic kidney disease: the way to improved clinical trial design and clinical practice? Kidney Int Rep. 2018; 4:212-221. doi: 10.1016/j.ekir.2018.12.001
Zewinger S, Rauen T, Rudnicki M, Federico G, Wagner M, Triem S, Schunk SJ, Petrakis I, Schmit D, Wagenpfeil S, Heine GH, Mayer G, Floege J, Fliser D, Gröne HJ, Speer T: Dickkopf-3 (DKK3) in urine identifies patients with short-term risk of eGFR loss. J Am Soc Nephrol. 2018; 29:2722-2733. doi: 10.1681/ASN.2018040405
Heinzel A, Kammer M, Mayer G, Reindl-Schwaighofer R, Hu K, Perco P, Eder S, Rosivall L, Mark PB, Ju W, Kretzler M, Gilmour P, Wilson JM, Duffin KL, Abdalla M, McCarthy MI, Heinze G, Heerspink HL, Wiecek A, Gomez MF, Oberbauer R: Validation of plasma biomarker candidates for the prediction of eGFR decline in patients with type 2 diabetes. Diabetes Care. 2018; 41:1947-1954. doi: 10.2337/dc18-0532
Pircher C, Schneeberger S, Boesmueller C, Agaimy A, Zoller H, Bale R, Henninger B, Mayer G, Neuwirt H: A rare case of Epstein-Barr virus-associated hepatosplenic smooth muscle tumors after kidney transplantation. Transpl Infect Dis. 2018; 20:e12860. doi: 10.1111/tid.12860
Fanciulli A, Mayer G et al: Consensus statement on the definition of neurogenic supine hypertension in cardiovascular autonomic failure by the American Autonomic Society (AAS) and the European Federation of Autonomic Societies (EFAS): Endorsed by the European Academy of Neurology (EAN) and the European Society of Hypertension (ESH). Clin Auton Res. 2018; 28:355-362. doi: 10.1007/s10286-018-0529-8
Perco P, Mayer G: Endogenous factors and mechanisms of renoprotection and renal repair. Eur J Clin Invest. 2018; 48:e12914. doi: 10.1111/eci.12914
Koppelstaetter C, Kern G, Leierer G, Mair SM, Mayer G, Leierer J: Effect of cyclosporine, tacrolimus and sirolimus on cellular senescence in renal epithelial cells. Toxicol In Vitro. 2018; 48:86-92. doi: 10.1016/j.tiv.2018.01.004
Perco P, Heinzel A, Leierer J, Schneeberger S, Bösmüller C, Oberhuber R, Wagner S, Engler F, Mayer G: Validation of systems biology derived molecular markers of renal donor organ status associated with long term allograft function. Sci Rep. 2018; 8:6974. doi: 10.1038/s41598-018-25163-8
Eder S, Leierer J, Kerschbaum J, Rosivall L, Wiecek A, de Zeeuw D, Mark PB, Heinze G, Rossing P, Heerspink HL, Mayer G: A prospective cohort study in patients with type 2 diabetes mellitus for validation of biomarkers (PROVALID) – study design and baseline characteristics. Kidney Blood Press Res. 2018;43:181-190. doi: 10.1159/000487500
Selection of Funding
- Markus Pirklbauer:Österreichische Nationalbank Anniversary Fund (grant number 18362): Intradialytic calcium kinetics and cardiovascular risk in hemodialysis patients
- Andreas Kronbichler: Versus Arthritis 22927 Measuring immunocompetence by assessment of torque-teno virus levels in autoimmune diseases following initiation of immunosuppression
- Andreas Kronbichler:NIH/NIAID Immune Tolerance Network (EIN No. 81-0726604)
- Michael Rudnicki:ERA Per Med: PERSTIGAN ( No. ERAPERMED 2018-217)
- Gert Mayer:Innovative Medicines Initiative (grant number 115974): Biomarker enterprise to attack diabetic kidney disease (Beat-DKD)
- Gert Mayer:Coordinator: Horizon 2020 (grant number 848011): Drug combinations for rewriting trajectories of renal pathologies in type II diabetes mellitus (DC-ren)
- Sara Denicolo: Multi-omics Signatur der Nierenfibrose bei CKD (KidneySign) (FWF Projekt I 6470 Internationale Projekte)
- Gert Mayer: Proteomische Signaturen für personalisierte Interventionen (SIGNAL) (FWF Projekt I 6471 Internationale Projekte)
- Philipp Gauckler: Land Tirol (F.35505): „Mobile application for real-time surveillance of endurance athletes“
Collaborations
- Heerspink Hiddo, University Medical Center Groningen, The Netherlands
- Ibberson Mark and Burdet Frederick, Swiss Institute of Bioinformatics, Lausanne, Switzerland
- Jayne David, University of Cambridge, United Kingdom
- Kotanko Peter, Renal Research Institute, New York, USA
- Schappacher-Tilp Gudrun, Joanneum Research
- Kretzler Matthias and Ju Wenjun, University of Michigan, Ann Arbor, USA
- Lancet Doron and Fishilevich Simon, Weizmann Institute of Science, Rehovot, Israel
- Mayer Bernd and Lukas Arno, emergentec biodevelopment GmbH Vienna, Austria
- Mischak Harald, Mosaiques Diagnostics GmbH, Hannover Germany
- Oberbauer Rainer and Heinzel Andreas, Medical University of Vienna, Vienna, Austria
- Poli Irene and Silvestri Claudio, European Center for Living Technology, Ca` Foscari University of Venice, Venice, Italy
- Rossing Peter, STENO Diabetes Center, Copenhagen, Denmark
- Jayne David, University of Cambridge, Cambridge, UK
- Stone John, Massachusetts General Hospital, Boston, USA
- The Department has established a biobank of several hundred thousand samples of different body fluid matrices and kidney biopsies. The patients included suffer from CKD, DKD and end stage renal disease (dialysis and transplantation).
- We execute mRNA microarray protocols for large-scale analysis of gene-expression in various samples. Genome wide gene expression profiling is combined with state-of-the-art methods such as qPCR, immunohistology, in situ hybridisation, western blotting and ELISAs to evaluate candidate genes and proteins using equipment like GenePix 4000B, Quantstudio 5, Olympus VS120 or Tecan Spark or MESO QuickPlex SQ 120MM.
- We manipulate in vitrogene- and protein expression, respectively, using CRISPR/Cas to analyse cellular functions.
- We use state of the art bioinformatics, statistics and data science tools to analyse expression profiles and run network/network interference analysis.