Anichstraße 35
6020 Innsbruck
Fax: +43 512 504 22824
Email: rohit.arora@i-med.ac.at
Website: https://ortho-trauma-innsbruck.tirol-kliniken.at/
Research Branch (ÖSTAT Classification)
102001, 104026, 106013, 106022, 106049, 206001, 211904, 301103, 301105, 301107, 301304, 301305, 301902, 301904, 302019, 302029, 302048, 302055, 302057, 302085, 303020, 304002, 305103, 305104, 305106, 305109, 305905, 305908, 601026
Keywords
arthroplasty, biofilm genetics, biomechanics, Cell biology, Clinical studies, fracture fixation, implant-related infections, microstructural bone failure, minimal-invasive surgery, and orthopaedics
Research Focus
Our research focuses on the evaluation, development and improvement of new and existing treatments for traumatic and degenerative musculoskeletal diseases throughout all disciplines: clinical randomised studies; biomechanical cadaver tests to improve implant behaviour; morphologic/cell biological investigations on aging processes and biofilm investigations regarding implant-related infections. Among others, 3D reconstruction, gait lab and micro CT allow us to research at the highest level.
General Facts
The department is organised into clinical teams specialising in anatomical regions. A networked infrastructure provides our clinicians with a wide ranging spectrum of research. This setting supports clinical research as wells as laboratory research at macroscopic, microscopic and cellular level. Clinical research mainly contains medical device studies and trials which explore treatment methods and its success, which is supported by our study coordination team. While our gait lab deals with movement analysis and optimisation, material testing machines are available for in vitro testing of soft and hard biological tissues in the biomechanics lab, with several custom-made test setups for various anatomical regions as well as joint simulators for the spine, knee, shoulder and hand. In addition biomedical engineering focuses on improving techniques for filling bony defects and bone removal. The morphology and cell biology investigations are based on intervertebral disc cell (IVD), especially on traumatised IVDs and IVDs obtained from patients with a degenerative disc disease. Osteoporosis and its underlying mechanisms are studied in a fully equipped tissue culture unit. The biofilm lab concentrates on implant-related infections studies aimed at the understanding of biofilm building and attachment on biomaterial surfaces. The two micro-CT scanners are used for scanner operations, image reconstruction, quantitative analysis, and 3D visualization.
Research
Clinical Research – Study Coordination
Mariëtte Fasser, MSc
The study coordination provides support in the organisation of clinical trials, ensuring a study planning and conduct according to local and international legal requirements. Furthermore, funding aspects, ethics committee submission, contract tracing and internal registrations are managed by the study coordination.
The majority of our trials are so called investigator initiated trials mostly funded by industry, public sponsor or foundation.
The main focus of our clinical studies is the continuous improvement of surgical and postoperative treatments, as well as the establishment of innovative devices or methods with the aim to reach permanent quality assurance and evidence-based medicine on the highest level.
With that mission in mind, best outcome for our patients is targeted and therefore research is performed especially on the musculoskeletal topics regarding fracture fixation, fracture reduction, prevention of implant failure, improvement of spinal cord injuries, joint arthroplasty, knee arthroscopy (cartilage repair) and return to sports.
This includes research questions such as: does optimal anatomical shape of medical devices obtain best functional outcome and cause less implant removals? Does a one-time shock wave application after acute spinal cord trauma surgery result in greater improvement in motor and sensory function?
In addition, basic clinical research investigates factors influencing an outcome and evaluates potential correlations that provide valuable information for future treatment recommendations.
Due to the departments, multifaceted research infrastructure and the study coordination as interface to regulatories and researchers, interdisciplinary as well as international collaborations can be enabled.
A joint project with the Institute of Hygiene and Medical Microbiology concentrates on the reduction of bacteria with the body-own antiseptic N-chlortaurine tested on anterior cruciate ligaments, prosthesis components and bovine tendons. The project was funded by the “Tiroler Wissenschaftsfond”; finalised in February 2023. N-chlorotaurine demonstrated a broad-spectrum bactericidal effect superior to the antibiotic comparator Vancomycin. Clinical benefit:
intraoperative antibiotic administration could be reduced, thus less risk of the development of resistance to antibiotics and broader spectrum of activity.
Currently, we are starting as a participating entity in a pharmaceutical study (Genera Res. Ltd) regarding locally administered treatment against Tibia Non-Union with Osteogrow-C (recombinant human bone morphogenetic protein 6 in Autologous Blood Coagulum) compared to bone autograft.
Furthermore, the secondary hip fracture prophylaxis is still a medical important focus which is investigated in a trial with the pharmaceutical sponsor AgNovos Healthcare. The concept of this study is calcium based bone cement (OSSURE LOEP) which is applied into the contralateral fragile hip, hardens intraoperatively and turns into bone after 5-7 years.
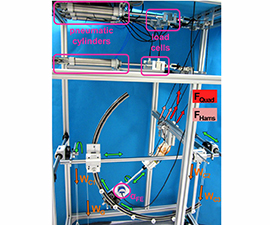
Biomechanics Laboratory
Werner Schmölz, Assoc. Prof., PhD, Dipl.-Ing (FH)
Implant anchorage in stabilisation procedures in patients having reduced bone quality still poses a challenge to the surgeons. Therefore, new test setups, loading protocols as well as algorithms to detect implant loosening during dynamic loading were developed and applied. With these developed tools, implant anchorage was investigated in various anatomical regions for different augmentation techniques and augmentation materials and surgical techniques. For the shoulder joint, we applied these tools to demonstrate that a mushroom shaped allograft in combination with a locking plate significantly enhances construct stiffness and failure load in patients with proximal humerus fractures and compromised bone quality and can therefore be a viable option for surgical treatment of unstable varus displaced proximal humerus fractures.
For the treatment of spinal pathologies, we investigated various instrumentations and surgical techniques on the biomechanics of the spine. For reduced bone quality, cement augmentation of pedicle screws to improve screw anchorage is an established procedure. However, each augmented screw also increases the risk of complications. We could show that augmentation of only the four marginal screws provides sufficient anchorage in long instrumentations,, while minimising the risk of PMMA augmentation complications. Regarding pedicle screw anchorage, we could confirm that – compared to ideal placed pedicle screws – lateral misplaced pedicle screws have a negative effect on screw anchorage. However, redirection if the misplaced pedicle screw does not improve, but rather compromises screw anchorage and may not be desirable if the misplaced screw does not harm relevant anatomical structures.
For the reconstruction of transverse acetabular fractures, different fixation techniques were compared under single leg stance and sit to stand loading. For clinical practice, our results showed that a single plate might not provide adequate stability for transverse fractures and should be complemented by an additional plate or a column screw. Furthermore, biomechanical testing of acetabular fracture fixation constructs should also include sit to stance loading, because the strength of the osteosynthesis is overestimated if only single leg stance loading is applied.
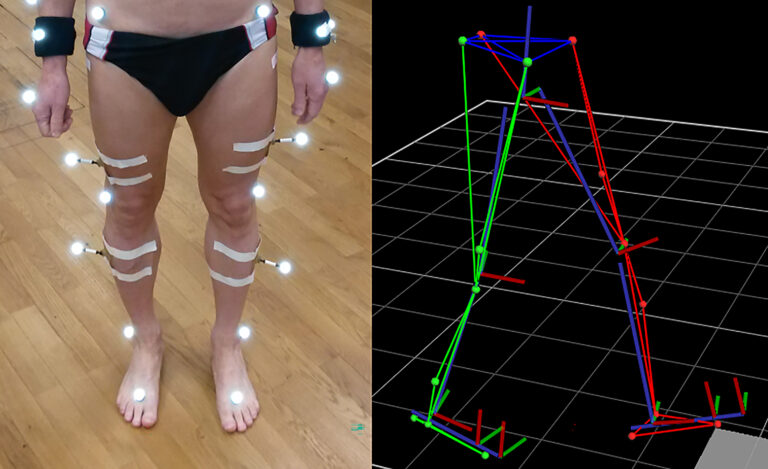
In ligamentous injuries of the knee, a lateral extra articular tenodesis (LET) can be performed additional to an anterior cruciate ligament reconstruction (ACLR). The LET is intended to reduce ACLR loading, prevent ACLR ruptures and restore knee kinematics. In an in vitro study applying a knee joint test bench (figure 1) we could demonstrate that anterior cruciate ligament reconstruction (ACLR) graft forces under internal tibia torque loading can be reduced with an additional lateral extra articular tenodesis (LET) and residual rotational laxity after isolated ACLR can be decreased. This might reduce the risk of ACLR re-ruptures, in particular for pivoting motions.
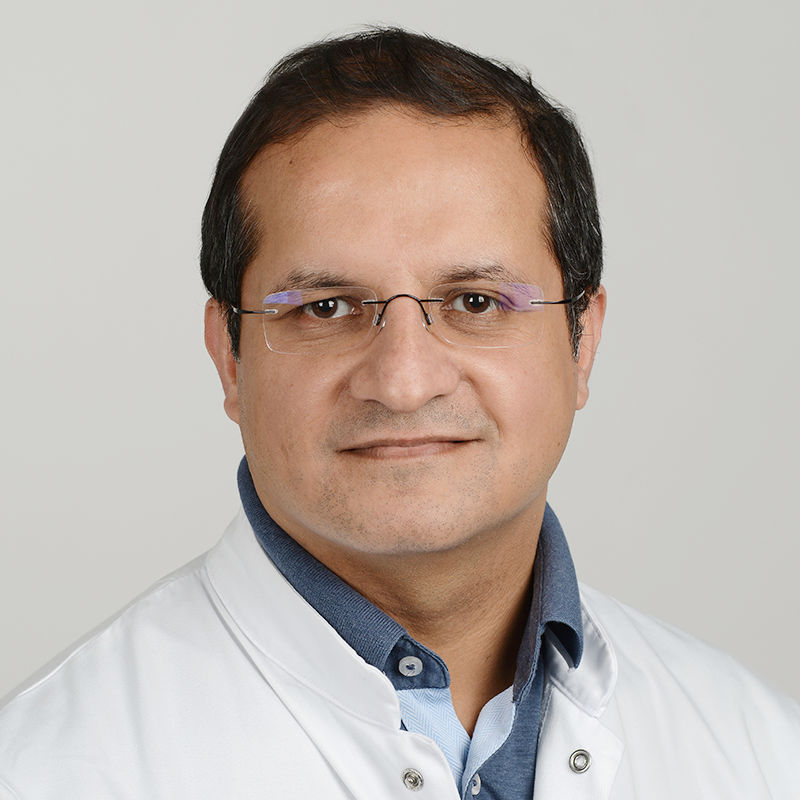
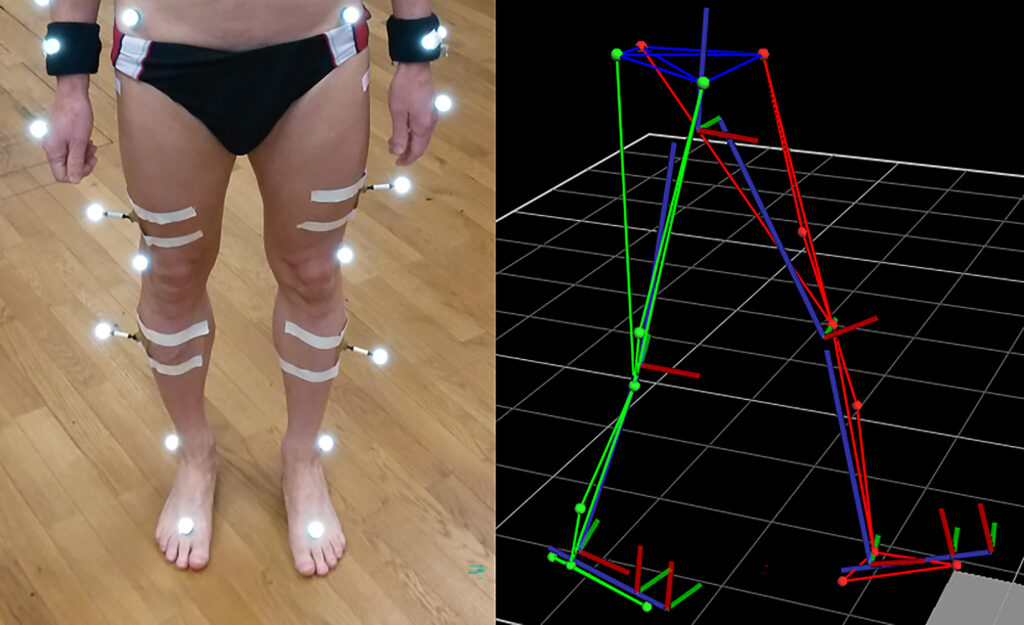
Orthopaedic Gait lab
Dipl. Ing. Stefan Fischler
Basically the research at the biomechanical gait lab focuses on movement analysis and movement optimisation. Within clinical trials, the instruments of the gait lab can be used to detect unhealthy loading or demonstrates differences in gait speed.
A Vicon system is used to analyse everyday movements and collect important information to improve ergonomic behaviour. The Vicon system consists of a Vicon MX Giganet with 8 infrared cameras, 2 colour cameras 720p and 2 pressure plates. Vicon Nexus 2 serves as recording and evaluation software (figure 2).
Current studies focus on the movement behaviour, for example, before and after knee surgery (e.g. arthroplasty, trochleoplasty) by determining all possible changes in the range of motion to investigate the best postoperative outcome between various treatment methods or implants. Among other things, the change in knee angle is determined and the measured ground reaction forces are compared.
The change in the patients’ mobility is also determined at scoliosis operations. Again, the range of motion (total angle of rotation between hip and torso) is of special interest and the change in mobility of the spine before and after surgery. The gained knowledge can lead to the optimisation of the therapy and merge into the clinical routinal patient care.
Morphology and Cell Biology – Intervertebral disc investigations
PD Dr. med. Ingrid Sitte, Miranda Klosterhuber BMA
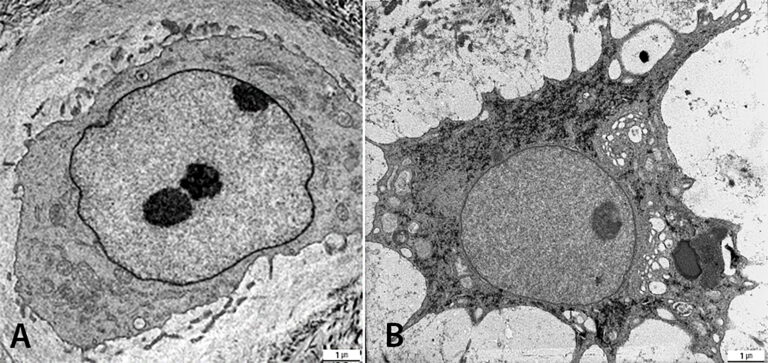
Traumatised IVDs of the cervical spine are studied histologically by light microscopy and ultra-structurally by transmission electron microscopy (TEM). The group investigates with regard to two parameters: fracture mechanism (compression vs. rotation fractures) and degeneration grade (low vs. high). Disc architecture is studied histologically. Cell morphology is examined ultra-structurally to quantify cell-death and healthy cells. According to ultrastructural observations, two time-groups (up to 6 days vs. later) are investigated. The degenerative disc diseases presented a new disc cell morphology, the balloon cell, which we first detected by Transmission Electron Microscopy. The goal is to examine this special cell in detail. These cells seem to be part of aging processes as well in the IVD, cartilage and adjacent bone structures. Moreover, our group studies intervertebral disc cells of the degenerated cervical spine with prolapse or protrusion and of the cervical spine post trauma in cell culture to analysis cell morphology and pro-inflammatory and pro-apoptotic proteins with special regard on the balloon cells. Whereas these cells in the disc matrix were obvious with mean 40%, cell culture presented up to 98% balloon cells in the degenerated herniated disc. Moreover, this special cell morphology, the balloon cell, present with diminished SPARC (Osteonectin) especially in the nucleus of human cells and cells gained from SPARC Null KO mice (figure 3). This may have an impact on an upcoming therapy.
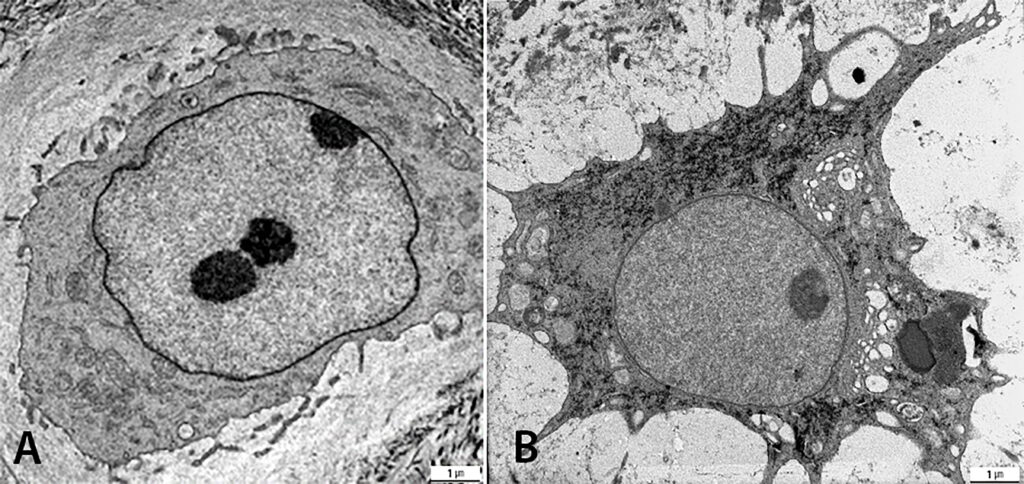
prolapsed disc (B): Both Balloon cells at a magnification of 4000x, presenting mostly euchromatin and
a nucleulus in the nucleus which is enveloped by an osmiophilic nucleus membrane
(Copyright: PD Dr. Ingrid Sitte – MUI )
Biofilm Lab – Implant-related infections
Ass. Prof. Dr. Deborah Coraça-Huber, PhD, MMSc
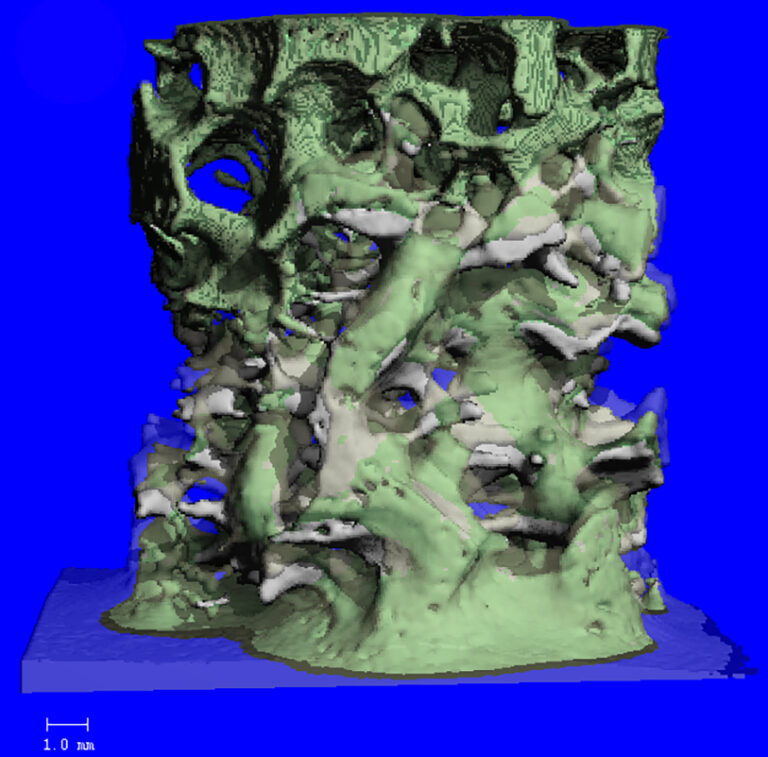
Improved understanding of the structure and function of biofilms (figure 4) help to develop treatments to avoid infections, develop new diagnostic tools as well as treat infections.
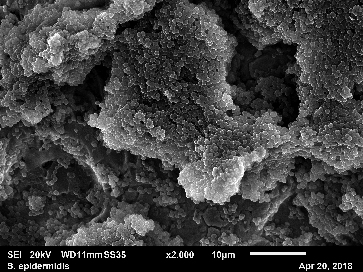
Biofilms-specific genes and the diagnosis of PJIs
A staphylococcal bacterial biofilm is produced in a two-step process: initial bacterial attachment to the surface of a foreign body or host tissue followed by a biofilm formation, consisting of bacterial proliferation, intercellular adhesion, and extracellular slime substance production. Different genes are involved in each phase of the biofilm formation. These biofilm-specific markers can be detected by feasible molecular methods.
Osseo integration of titanium implants aiming biofilm prevention and peri-implantitis prevention.
An interdisciplinary project involving dental medicine and orthopaedics has been carried out, aiming the development of a titanium surface capable of avoiding the attachment of bacteria and biofilm formation. The results obtained in this study will be translated to the orthopaedic area.
Natural antimicrobial substances
Instead of developing new antibiotics, there is the need to investigate alternative and antibiotic boosting substances. Alternative substances can be administered alone, locally, for the treatment of wound infections and implant infections. In addition, such substances can act as coadjutants increasing the activity of systemically applied antimicrobials.
Metagenomics Sequencing
The use of the new technology using a metagenomics Oxford Nanopore Sequencing tool enable us to detect microbial population in different substrates, as human fluids like joint aspirates, biopsies, sonication fluids. Together with the capacity of this method to detect antibiotic resistance genes, the use of this new technology can help develop new diagnostic tools for PJI.
Biofilm-related Oncogenesis
Biofilms, once in contact with human tissue can lead to inflammation which can lead to oncogenesis. The biofilm-related oncogenesis can develop in several tissues and systems. Mostly studies is the oncogenesis of colon carcinoma after the transition of a healthy microbiome in a pathogenic form of biofilm. The knowledge obtained from this area can help in the investigation of bone tissue cancer and its probable relation to a prior infection and biofilm formation.
PD David Putzer, PhD, MSc
Bone transplants
Bone chips are used in many fields to reconstruct bone defects and to act as a filling material for bone defects. Bone defects often have a multifactorial genesis. Especially when removing bone tumours, in cranio-maxillofacial interventions and in the revision of total hip arthroplasties, bone defects can be generated that subsequently might require treatment. Bone grafting is a surgical technique to fill in bone defects by replacing it with autogenous, allogeneic or artificial bone-material.
Impaction forces and its effects on the human body
The surgeon’s feeling when broaching the femoral canal or the force necessary for proper impaction of the hip or knee implant varies depending on different tools and different tissues. Especially when implanting an acetabular cup, the least possible force required for impaction should be determined and analysed for different bone qualities to increase safety and avoid fractures in hip surgeries. Similar fixation techniques are also used in the knee and shoulder and most of the impaction processes are not standardised.
Radial shockwave therapy is used for therapeutic purposes. Also in this case, little is known on the effects on the tissue of the mechanical impacts during shockwave therapy.
Implant migration
When analysing the follow up X rays of patients, implant migration can be assessed using the EBRA technique. Assessing implant migration is necessary to predict early implant failure and to investigate possible design effects of different implant systems. Currently, a mathematical correlation model is being developed in predicting wear behaviour in different patients based on plane X-rays.
Robotic assisted surgery
The effects of robotic assisted surgery on the surgical workflow as well as for the outcome of the patients are necessary to evaluate the cost/benefit ration of such systems. Particularly the early adoption phase is of special interest, as it is a challenge for the entire surgical team. In this study, we evaluate the physical and mental stress as well as the learning curves when using the MAKO system.
Enhancing bone cement properties
Bone cement has been used in surgical fixation of artificial joints. The primary function of bone cement is to transfer forces from bone to prosthesis and the long-term success of a total joint prosthesis depends on it. The presence of voids reduces the fracture resistance of bone cement. We investigate in reinforcement strategies using wires or adding components such as carbons. Beside the primary function to act as fixation material, bone cement can also be used to transfer antibiotics during the treatment of implant associated infections. The alteration of the mechanical properties is evaluated when adding antibiotic components to the bone cement.
Core facility – Micro CT
PD MMag. Dr. Pallua Johannes, MSc PhD
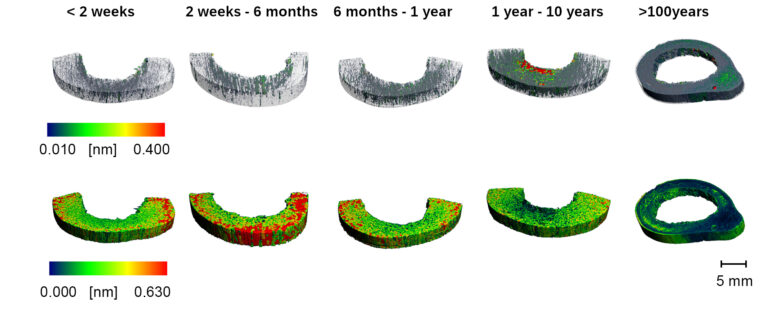
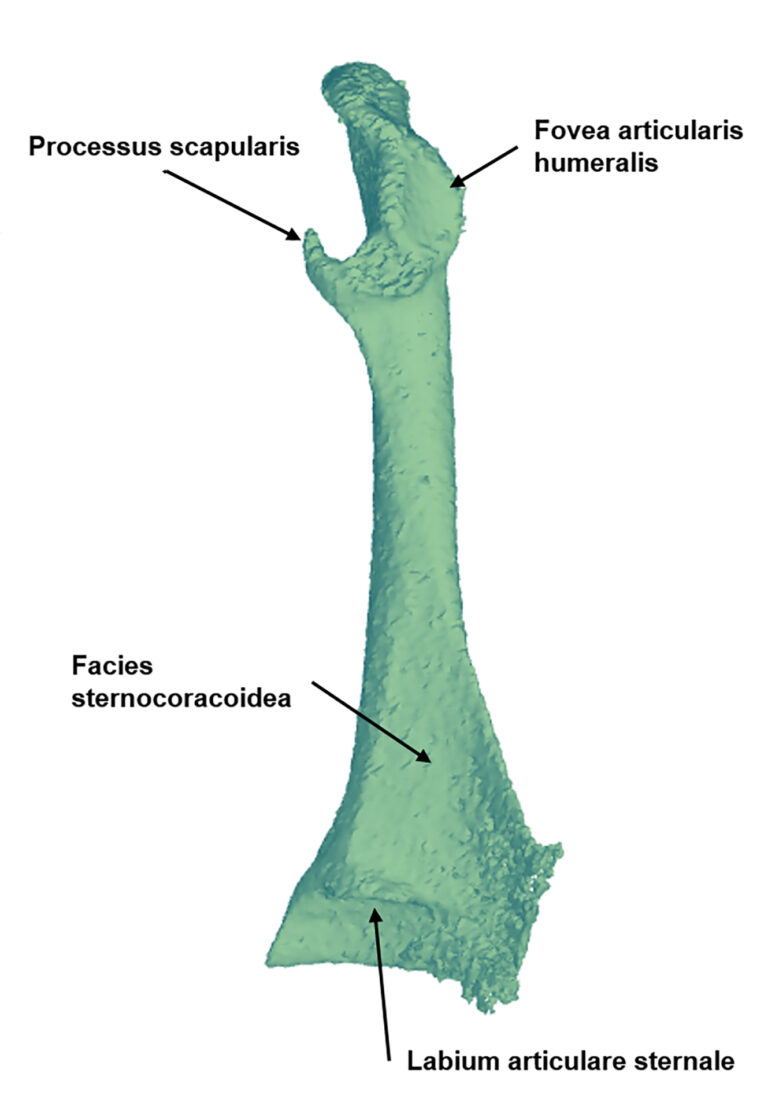
Micro-CT is an X-ray imaging technique that non-destructively assesses various high-resolution materials, including musculoskeletal tissues and biomaterials. This technique has many research applications, such as analysing fracture healing, evaluating skeletal phenotypes, repairing segmental bone defects, investigating age-related effects on bone, studying joint degeneration, exploring vascular remodelling, delving into developmental biology and examining the microstructure of materials. (fig. 5-7)
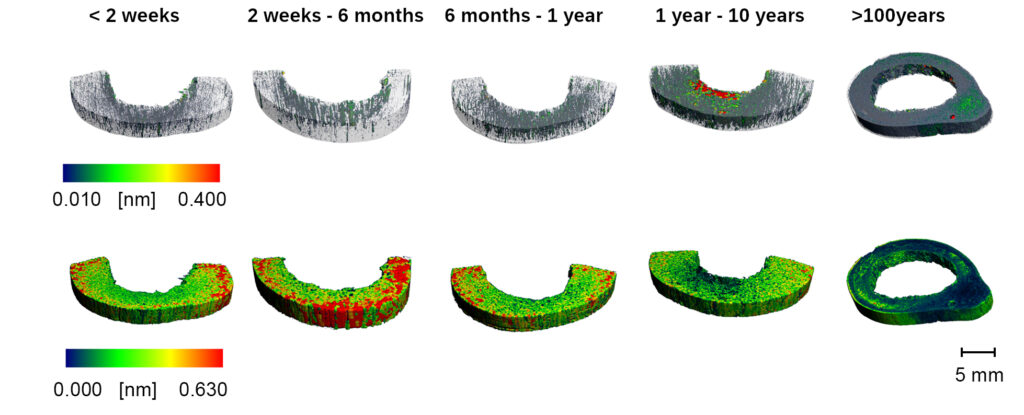
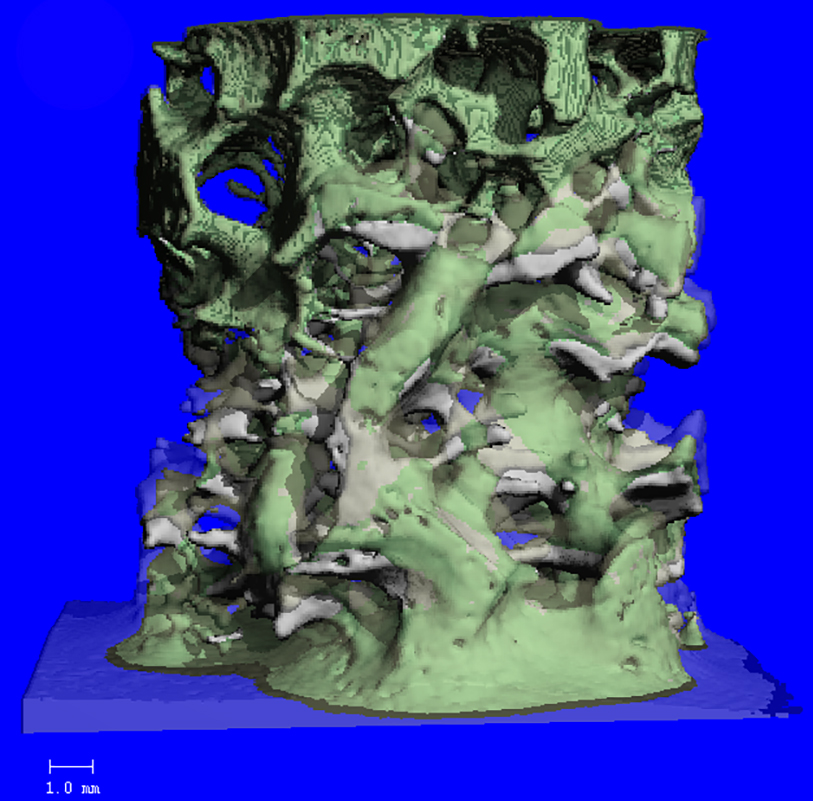
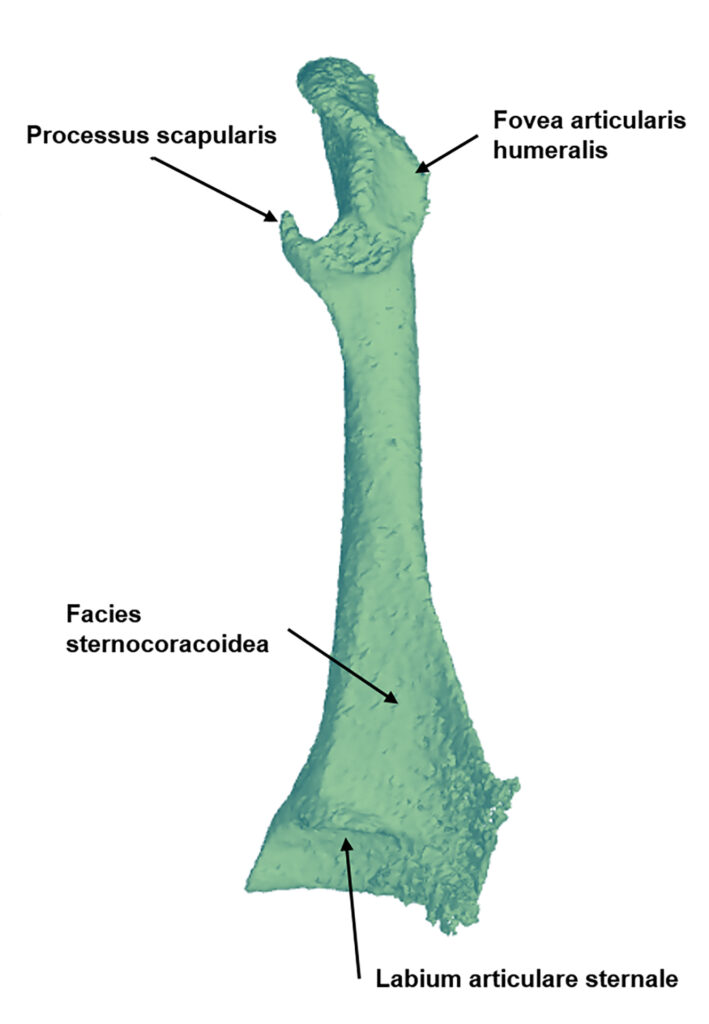
The Core facility micro-CT houses two micro-CT systems and a cluster of workstations used for scanner operations, image reconstruction and quantitative analysis, and 3D visualisation. The Scanco vivaCT 40 has a maximum field of view of 38mm diameter and can image live rodents and ex vivo specimens at 10-38 µm voxel resolutions. The XtremeCTII is used for high-resolution scanning of the extremities of patients, mainly for the evaluation of bone density and micro-architecture, e.g. in the scaphoid bone. The power of these systems lies in their ability to extract quantitative morphometric and density data and 3D models of specimens, enabling researchers to explore a wide range of applications.
3D models can benefit numerous applications such as telemedicine or surgery planning and patient education. Today’s state-of-the-art technology allows patient-specific 3D models to be created from computed tomography, magnetic resonance imaging or 3D ultrasound data using special segmentation software. These 3D models can then be printed in their original size using a 3D printer, resulting in a lifelike representation of the patient’s anatomy or pathology. As part of our work at the Univ. Clinic for Orthopedics and Traumatology, we support:
- the segmentation of medical images
- the creation of 3D models
- intervention planning and visualization
- printing of 3D anatomical models for manual adjustment of surgical plates
- the performance of virtual surgeries or important measurements
- the production of patient-specific templates
Pictures
Selected Publications
CLINICAL STUDIES:
Atkins PR, Stock K, Ohs N, Collins CJ, Horling L, Benedikt S, Degenhart G, Lippuner K, Blauth M, Christen P, Müller R. Formation Dominates Resorption With Increasing Mineralized Density and Time Postfracture in Cortical but Not Trabecular Bone: A Longitudinal HRpQCT Imaging Study in the Distal Radius. JBMR Plus. 2021 Apr 8;5(6):e10493. doi: 10.1002/jbm4.10493. eCollection 2021 Jun.PMID: 34189382
Kosiol, Juana; Keiler, Alexander; Loizides, Alexander; Gruber, Hannes; Henninger, Benjamin; Bölderl, Andreas; Gruber, Leonhard: Operative versus conservative treatment of acute Achilles tendon ruptures: preliminary results of clinical outcome, kinematic MRI and contrast-enhanced ultrasound. ARCHIVES OF ORTHOPAEDIC AND TRAUMA SURGERY. 2022; [Epub ahead of print]
Stock K, Benedikt S, Kastenberger T, Kaiser P, Arora R, Zelger P, Pallua JD, Schmidle G. Outcomes of distal ulna locking plate in management of unstable distal ulna fractures: a prospective case series. Arch Orthop Trauma Surg. 2022 Jul 18. doi: 10.1007/s00402-022-04549-4. Online ahead of print.PMID: 35849186
Schneider F, Geir F, Koidl C, Gehrer L, Runer A, Arora R. Retrospective evaluation of radiological and clinical outcomes after surgical treatment of proximal femur fractures utilizing TFNA. Arch Orthop Trauma Surg. 2022 Dec 2. doi: 10.1007/s00402-022-04704-x. Epub ahead of print. PMID: 36456766.
BIOMECHANIC LAB:
Dankl, Lukas; Schmoelz, Werner; Hoermann, Romed; Euler, Simon: Evaluation of mushroom-shaped allograft for unstable proximal humerus fractures. ARCHIVES OF ORTHOPAEDIC AND TRAUMA SURGERY. 2022; 142(3); 409-416.
Schmoelz, Werner; Zierleyn, Jan Philipp; Hoermann, Romed; Arora, Rohit: Standardized fracture creation in the distal humerus and the olecranon for surgical training and biomechanical testing. ARCHIVES OF ORTHOPAEDIC AND TRAUMA SURGERY. 2022; 142(12); 3853-3861.
Mayr Raul, Sigloch Maximilian, Coppola Christian, Hoermann Romed, Iltchev Alesandra, Schmoelz Werner.: Modified Lemaire tenodesis reduces anterior cruciate ligament graft forces during internal tibial torque loading. JOURNAL OF EXPERIMENATL ORTHOPAEDICS of Experimental Orthopaedics. 2022 18;9(1):45. doi: 10.1186/s40634-022-00484-w.
Quang, Huy Le; Schmoelz, Werner; Lindtner, Richard A.; Dammerer, Dietmar; Schwendinger, Peter; Krappinger, Dietmar: Single column plate plus other column lag screw fixation vs. both column plate fixation for anterior column with posterior hemitransverse acetabular fractures – a biomechanical analysis using different loading protocols. INJURY-INTERNATIONAL JOURNAL OF THE CARE OF THE INJURED. 2021; 52(4); 699-704.
Ali, Athar; Fontanari, Vigilio; Fontana, Marco; Schmölz, Werner: Spinal Deformities and Advancement in Corrective Orthoses. BIOENGINEERING-BASEL. 2020; 8(1); 2.
BIOFILM LAB
Spiegel C, Nogler M, Coraça-Huber DC. Sterilization Procedures for Titanium Alloy Surfaces Leads to Higher Expression of Biofilm-Related Staphylococcus aureus Genes. Antibiotics (Basel). 2022 Nov 17;11(11):1647. doi: 10.3390/antibiotics11111647. PMID: 36421291; PMCID: PMC9686690.
Spiegel C, Steixner SJM, Coraça-Huber DC. Antibiofilm Activity of Omega-3 Fatty Acids and Its Influence on the Expression of Biofilm Formation Genes on Staphylococcus aureus. Antibiotics (Basel). 2022 Jul 11;11(7):932. doi: 10.3390/antibiotics11070932. PMID: 35884185; PMCID: PMC9311851.
Coraça-Huber DC, Steixner S, Wurm A, Nogler M. Antibacterial and Anti-Biofilm Activity of Omega-3 Polyunsaturated Fatty Acids against Periprosthetic Joint Infections-Isolated Multi-Drug Resistant Strains. Biomedicines. 2021 Mar 26;9(4):334. doi: 10.3390/biomedicines9040334. PMID: 33810261; PMCID: PMC8065983.
Steixner SJM, Spiegel C, Dammerer D, Wurm A, Nogler M, Coraça-Huber DC. Influence of Nutrient Media Compared to Human Synovial Fluid on the Antibiotic Susceptibility and Biofilm Gene Expression of Coagulase-Negative Staphylococci In Vitro. Antibiotics (Basel). 2021 Jun 29;10(7):790. doi: 10.3390/antibiotics10070790. PMID: 34209737; PMCID: PMC8300679.
Grimus V, Coraça-Huber DC, Steixner SJM, Nagl M. Activity of N-Chlorotaurine against Long-Term Biofilms of Bacteria and Yeasts. Antibiotics (Basel). 2021 Jul 22;10(8):891. doi: 10.3390/antibiotics10080891. PMID: 34438941; PMCID: PMC8388722.
BONE TRANSPLANTS
Putzer D, Dammerer D, Huber C, Boschert H, Thaler M, Nogler M (2022) Aerosol morphology and particle size distribution in orthopaedic bone machining: a laboratory worst-case contamination simulation. Is high-speed bone machining potentially harmful by pollution and quality schemes and what measures could be taken for prevention? Int Orthop 46:1647-1655. DOI 10.1007/s00264-022-05398-x
Putzer D, Dammerer D, Baldauf M, Lenze F, Liebensteiner MC, Nogler M (2022) A Prospective Assessment of Knee Arthroscopy Skills Between Medical Students and Residents-Simulator Exercises for Partial Meniscectomy and Analysis of Learning Curves. Surgical innovation 29:398-405. DOI 10.1177/15533506211037792
Pallua JD, Putzer D, Jager E, Degenhart G, Arora R, Schmolz W (2022) Characterizing the Mechanical Behavior of Bone and Bone Surrogates in Compression Using pQCT. Materials (Basel) 15. DOI 10.3390/ma15145065
Dammerer D, Blum P, Putzer D, Krappinger D, Liebensteiner MC, Nogler M, Thaler M (2022) Subsidence of a metaphyseal-anchored press-fit stem after 4-year follow-up: an EBRA-FCA analysis. Arch Orthop Trauma Surg 142:2075-2082. DOI 10.1007/s00402-021-04068-8
Putzer D, Coraca-Huber D, Huber C, Boschert H, Thaler M, Nogler M (2021) The spatial distribution of aerosols in high-speed bone burring with external irrigation. J Microbiol Methods 184:106205. DOI 10.1016/j.mimet.2021.106205
MICRO-CT/3D-Reconstruction:
H. Unterberger, C. Berger, M. Schirmer, A. K. Pallua, B. Zelger, G. Schäfer, C. Kremser, G. Degenhart, H. Spiegl, S. Erler, D. Putzer, R. Arora, W. Parson and J. D. Pallua: Morphological and Tissue Characterization with 3D Reconstruction of a 350-Year-Old Austrian Ardea purpurea Glacier Mummy Biology (2023): 10.3390/biology12010114
Benedikt, L. Horling, K. Stock, G. Degenhart, J. D. Pallua, G. Schmidle, R. Arora: The impact of motion induced artifacts in the evaluation of HR- pQCT scans of the scaphoid bone: an assessment of inter- and intraobserver variability and quantitative parameters. QIMS (2022): 10.21037/qims-22-345
M. Schmidt, P. Zelger, C. Woess, A. K. Pallua, R. Arora, G. Degenhart, A. Brunner, B. Zelger, M. Schirmer, W. Rabl, J. D. Pallua: Application of Micro-Computed Tomography for the Estimation of the Post-Mortem Interval of Human Skeletal Remains. Biology (2022): 10.3390/biology11081105.
D. Pallua, D. Putzer, E. Jäger, G. Degenhart, R. Arora, W. Schmölz: Characterizing the Mechanical Behavior of Bone and Bone Surrogates in Compression Using pQCT. Materials (2022): 10.3390/ma15145065.
A.Wurm, J.Kühn. K.Kugel, D.Putzer, R.Arora, D.C.Coraça-Huber, P. Zelger, J.Badzoka, C.Kappacher, C.W.Huck, J.D.Pallua: Raman microscopic spectroscopy as a diagnostic tool to detect Staphylococcus epidermidis in bone grafts. Spectrochimica Acta Part A: Molecular and Biomolecular Spectroscopy (2022): 10.1016/j.saa.2022.121570
Selection of Funding
Clinical Studies:
AgNovos Healthcare Sponsoring – RESTORE project OSSURE LOEP
Genera Sponsoring Tibia Non-Union Prject
IIT Grant DePuySynthes/Johnson&Johnson
IIT Grant Medacta International
IIT Grant Medartis
AO Trauma Austria Grant
Biomechanic Lab:
MedTech Industry
Deutsche Wirbelsäulenstiftung (DWS)
Gesellschaft für Orthopädisch-Traumatologische Sportmedizin (GOTS)
Tiroler Wissenschaftsfond
AO Austria
Biofilm Lab:
IRASME – DIAMOND Project 2022
Ffg Praktika 2021, 2022, 2023
Bone Transplants
FFG Praktika 2021
Collaborations
Clinical Studies:
Department of Otorhinolaryngology Innsbruck
Department of Physical Therapy Innsbruck
Institute of Hygiene and Medical Microbiology Innsbruck
Medartis AG, Basel, Switzerland
Medacta International SA, Castel San Pietro, Switzerland
AO Trauma Austria
Genera Research Ltd, Kalinovica, Croatia
Biomechanic Lab:
Prof. Dr. med. Tobias Schulte, University of Munster, Germany
Prof Dr. med Heiko Koller, TU Munich, Klinikum Rechts der Isar, Germany
PD Dr. med Sven Märdian, Charite, Berlin, Germany
Luis Alvarez Galovic, Hospital Universitario Fundacion Jimenez Diaz, Madrid, Spain
Prof. Vigilino Fontanari, Department of Industrial Engineering, University of Trento, Trento, Italy
Prof. Marco Fontana, Institute of Mechanical Intelligence, Scuola Superiore Sant’Anna, Pisa, Italy
Prof. Dr.. med Yu-Mi Ryang, Neurosurgery, Helios Klinikum Berlin-Buch, Germany
Prof. Dr. med. Jürgen Harms, Heidelberg, Germany
Prof. Dr.-Ing. Sebastian Dendorfer and Prof. Dr.-Ing Lars Krenkel, OTH Regensburg, Germany
Prof. Dr. Felix Capanni, University of Applied Science Ulm, Germany
Prof. Dr. Steffen Wolf, Hochschule Offenburg, Germany
Ass. FH-Prof Dr. Dipl.-Ing Daniel Sieber, MCI, Innsbruck
Biofilm Lab:
AdvantIQX Implants, Gersthofen, Germany
Heraeus Medical GmbH, Wehrheim, Germany
Cell and Tissuebank Austria (CTB-A), Krems an der Donau, Austria
Bone Transplants
Politecnico di Torino, Torino, Italy
Technische Universität München, München, Germany
Stryker Leibinger GmbH, Freiburg, Germany
Head GmbH, Bregenz, Austria
Micro-CT/3D Reconstrucion:
Harald Spiegl and Simon Erler WESTCAM Datentechnik GmbH, Gewerbepark 38, 6068 Mils, Austria
Etienne Bechtel and Andreas Stahl Spectral Engines GmbH, Weißkirchener Straße 2-6, 61449 Steinbach, Germany
Christian Huck, Institute of Analytical Chemistry and Radiochemistry, Innrain 80-82, 6020 Innsbruck, Austria
Seraphin Unterberger, Institute of Material-Technology, Leopold-Franzens University Innsbruck, Technikerstraße 13, 6020 Innsbruck, Austria
Roland Stalder, Institute of Mineralogy and Petrography, Leopold-Franzens University Innsbruck, Innrain 52 6020 Innsbruck, Austria