
Fax: +43 512 504 27453
Email: claudius.thome@i-med.ac.at
Website: https://neurochirurgie.tirol-klinken.at/
Research year
Research Branch (ÖSTAT Classification)
302051, 303026, 303040, 302069, 302058, 302048, 302043, 302009, 302031, 302047, 302055, 302056
Keywords
functional neurosurgery, neurointensive care, neurooncology, neurotrauma, neurovascular, pediatric neurosurgery, regenerative medicine, spinal cord injury, and spine surgery
Research Focus
We actively host investigator-driven academic studies and participate in multinational trials in different fields of our practice. In our laboratory, clinical research operates in parallel with experimental work. We pursue the idea of taking innovative concepts from “bench to bedside”. In addition to ongoing research into tumour cell communication and spinal regeneration and biomechanics, we have conducted various investigations into the prevention of vasospasm after intracranial bleeding. Our main research focuses are divided into specialist groups.
General Facts
The Department of Neurosurgery has a total of 73 beds, including a neurosurgical critical care unit (10 fully ventilated beds, 3 intermediate care beds), and 4 permanent state-of-the-art operating theatres. These are equipped with intraoperative imaging (CT and ultrasound), neuronavigation, robotic microscopes (including intraoperative fluorescence techniques) and intraoperative neurophysiological monitoring devices.
The department acts as a referral centre for the entire spectrum of neurosurgical diseases, encompassing the territory of the state of Tyrol and neighbouring areas. Furthermore, the department receives referrals on a nationwide scale when second opinions and specialist therapeutic procedures are required.
The Departments of Neurology, Neuroradiology, Radiation Oncology, Psychiatry and Medical Oncology represent key collaborations in the field of the clinical routine (including joint programmes).
Research
Neuro-Oncology and Neurosurgical Oncology
Investigators: PD Dr. C.F. Freyschlag, Dr. J. Kerschbaumer, PhD, Dr. D. Pinggera, PhD;
The neuro-oncology programme is involved in international clinical research, including phase-II and III trials for the adjuvant treatment of gliomas. Most gliomas fulfil international criteria for “rare diseases” and this highlights the need for research networks. The neuro-oncology team is involved in networks and trials, including the European Low-Grade Glioma Network (ELGGN), the EORTC, the German Society for Neurosurgery (DGNC) and the EANS.
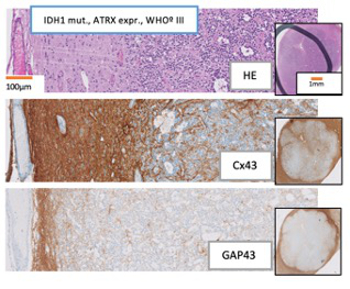
Experimental investigations into the infiltration of brain metastases and gliomas are ongoing with respect to cell-cell communication (Fig. 1) and microRNA. Active collaborations include with the Department of Neuroradiology on the evaluation of brain metabolism using phosphorus-31 MR spectroscopy and with the Department of Neurology in respect of the adjuvant treatment of gliomas and the neuropsychological evaluation of patients undergoing surgery for eloquent tumours. Operative visualisation techniques are currently under investigation; fluorescence-guided resections, digital visualisation tools and intraoperative imaging with ultrasound and CT are being evaluated.
Selected trials:
- miRNA in tumour cell communication
- Connexin43 and GAP-43 in low-grade gliomas
- Postoperative radiotherapy in meningiomas (EORTC – ROAM study)
- Intraoperative imaging in brain tumour surgery
- Use of robotic microscopes in brain and skull base surgery
Spinal Surgery, Spinal Regeneration and Biomechanics
Investigators: Univ.-Prof. Dr. C. Thomé; PD Dr. S. Hartmann, PhD; PD Ing. Dr. D. Shenegelegn-Mern; PD Dr. O. Petr, PhD; Dr. P.-P. Girod
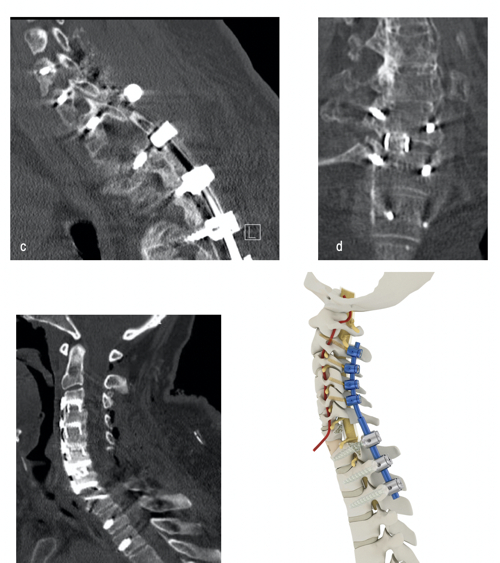
The spinal research team focuses on three fields of interest: improving clinical and functional patient outcome, experimental regenerative attempts, and biomechanical investigations into spinal pathologies (Fig. 2). We have also conducted experimental studies to elucidate the benefits of therapeutic approaches for intervertebral disc diseases with a self-complementary adeno-associated virus-mediated knockdown of specific gene loci (ADAMTS4). Our experimental laboratory focuses on regenerative attempts to improve therapeutic strategies.
Minimal invasive surgery using state-of-the-art neuronavigation systems and imaging technology is another clinical research interest. As well as taking part in a prospective multicentre study (EUROSPIN) to evaluate the accuracy of pedicle screw placement using a “free-hand”, a navigated or robot-guided technique, we are involved in an international, multicentre machine learning (ML) algorithm for outcome prediction after lumbar spinal fusion, with the aim of development and external validation of a robust prediction tool.
Additionally, the treatment options of complex spine instrumentations in the case of cervical deformities, neoplastic infiltrations or infectious diseases are being investigated biomechanically, in collaboration with the biomechanical laboratory of the Department of Orthopaedics and Traumatology.
Selected trials:
- Early surgery determines the recovery of motor deficits in lumbar disc herniations – a prospective single-centre study.
- The influence of surface EMG-triggered multichannel electrical stimulation on sensomotoric recovery in patients with lumbar disc herniation: A study protocol for a randomised controlled trial (RECO).
- Development and external validation of an international, multicentre, machine-learning algorithm to predict outcome after lumbar spinal fusion for degenerative disease: The FUSE-ML Study.
- SAMA trial: A database of adult spinal deformity.
- Self-complementary adeno-associated virus serotype 6 mediated knockdown of ADAMTS4 induces long-term and effective enhancement of aggrecan in degenerative human nucleus pulposus cells: A new therapeutic approach for intervertebral disc disorders.
- Animal models of regenerative medicine for biological treatment approaches to degenerative disc diseases.
- APOE-knockout in rabbits causes loss of cells in nucleus pulposus and enhances levels of inflammatory catabolic cytokines, damaging the intervertebral disc matrix.
- A scoring system for the preoperative evaluation of prognosis in spinal infection: The MSI-20 Score.
- Early decompression (<8 hours) improves functional bladder outcome and mobility after traumatic thoracic spinal cord injury.
- Surgical nuances and construct pattern influence construct stiffness in C1-2 stabilisations: A biomechanical study of C1-2 gapping and advanced C1-2 fixation.
- Biomechanical investigation of lumbar hybrid stabilisation in two-level posterior instrumentation.
Functional Neurosurgery and Pain Therapy
Investigators: Univ.-Prof. Dr. W. Eisner
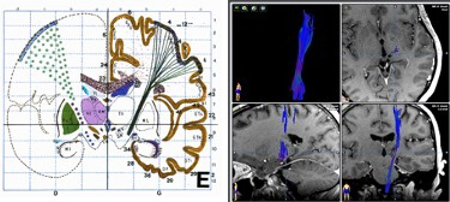
Functional neurosurgery is dedicated to the treatment of pharmacoresistant movement disorders, epilepsy, severe psychiatric disorders and chronic pain syndromes. The aim of the surgical discipline is to restore disturbed neuronal functionality by methods such as stereotactic surgery, radiosurgery, neuromodulation, functional imaging and intraoperative electrophysiology. The strong collaboration of neurology with neurosurgery has alleviated the Innsbruck experience of movement disorders and gained an international reputation. More than 50 peer-reviewed articles have been published since 1999, including in the New England Journal of Medicine, The Lancet, Brain and several top-ranked journals in neurology and neurosurgery.
Functional neurosurgery lies at the centre of the discovery of cerebral functions by means of intraoperative examinations in awake surgeries. It pursues these findings in order to compare intraoperative findings and functional neuroimaging, to bridge the gap between human brain physiology, cognitive and emotional behaviour control, decision-making, communication and metaphysical experiences.
Selected trials:
- Long-term follow-up of deep brain stimulation in Parkinson’s disease.
- Long-term follow-up of deep brain stimulation in generalised dystonia.
- Long-term follow-up of deep brain stimulation in segmental dystonia.
- VERCISE-DBS registry.
- Deep brain stimulation in Huntington’s disease
- Central post-stroke pain and deep brain stimulation.
Vascular Neurosurgery / Neurointensive Care / Neurotrauma
Investigators: Univ.-Prof. Dr. C. Thomé, PD Dr. C.F. Freyschlag, PD Dr. C. Unterhofer; PD Dr. O. Petr, PhD.
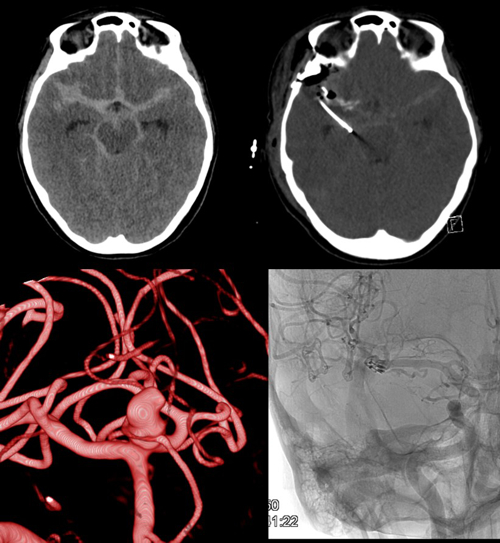
In addition to the continual prospective analysis of treatment results of vascular pathologies (e.g. aneurysms, arteriovenous malformations, arteriovenous fistulas, intracerebral haematomas and strokes etc.) and constant improvements in technical standards, adjuncts and operative techniques, the use of advanced imaging along with various biomarkers is being investigated, in order to have a beneficial influence on patient treatment and neurological outcome.
Severe head injury and aneurysmal SAH (Fig. 4) as well as haemorrhagic strokes are common medical conditions in the department. As well as multimodal monitoring and numerous pathophysiological investigations, various multi and monocentric studies are regularly undertaken. Invasive multimodal neuromonitoring of brain oxygenation, metabolism, blood flow and intracranial pressure alongside advanced imaging and targeted metabolomic profiling are performed for continuous evaluation of these techniques in treatment optimisation and patient outcome after subarachnoid haemorrhage and severe/moderate head trauma.
Selected trials:
- Dual ICP: Simultaneous application of multimodal invasive neuromonitoring in both intracranial supra/infratentorial compartments of patients with posterior fossa lesions, to obtain additional comprehensive data from the entire brain.
- NICAPLANT: Phase-IIb trial of nicardipine prolonged release pellets in aneurysmatic subarachnoid haemorrhage.
- TIBI I/II: Multimodal invasive neuromonitoring in patients with severe and moderate head trauma in combination with early MRI and targeted metabolomics, identifying CFS and serum biomarkers of neuronal injury.
- PREVAIL: Pilot trial of autologous intravenous CSF transfusion for the prevention of cerebral vasospasm after SAH.
- Cerebral vasospasm and delayed cerebral ischaemia after aneurysmal SAH – European / North American surveys and transnational cohort studies.
- German Cranioplasty Registry: Active participation in this bilateral register of patients undergoing cranioplasty after decompressive surgery.
Pictures
Selected Publications
Neurooncology and Neurosurgical Oncology
- Staartjes VE, Broggi M, Zattra CM, Vasella F, Velz J, Schiavolin S, Serra C, Bartek J Jr, Fletcher-Sandersjöö A, Förander P, Kalasauskas D, Renovanz M, Ringel F, Brawanski KR, Kerschbaumer J, Freyschlag CF, Jakola AS, Sjåvik K, Solheim O, Schatlo B, Sachkova A, Bock HC, Hussein A, Rohde V, Broekman MLD, Nogarede CO, Lemmens CMC, Kernbach JM, Neuloh G, Bozinov O, Krayenbühl N, Sarnthein J, Ferroli P, Regli L, Stienen MN; FEBNS. Development and external validation of a clinical prediction model for functional impairment after intracranial tumor surgery. J Neurosurg. 2020 Jun 12:1-8. doi:10.3171/2020.4.JNS20643. Epub ahead of print.
- Darlix, A.; Mandonnet, E.; Freyschlag, CF.; Pinggera, D.; Forster, MT.; Voss, M.; Steinbach, J.; Loughrey, C.; Goodden, J.; Banna, G.; Di Blasi, C.; Foroglou, N.; Hottinger, AF.; Baron, MH.; Pallud, J.; Duffau, H.; Rutten, GJ.; Almairac, F.; Fontaine, D.; Taillandier, L.; Pessanha Viegas, C.; Albuquerque, L.; von Campe, G.; Urbanic-Purkart, T.; Blonski, M.: Chemotherapy and diffuse low-grade gliomas: a survey within the European Low-Grade Glioma Network. NEURO-ONCOLOGY PRACTICE. 2019; 6(4); 264-273
- Klughammer J, Kiesel B, Roetzer T, Fortelny N, Nemc A, Nenning KH, Furtner J, Sheffield NC, Datlinger P, Peter N, Nowosielski M, Augustin M, Mischkulnig M, Ströbel T, Alpar D, Ergüner B, Senekowitsch M, Moser P, Freyschlag CF, Kerschbaumer J, Thomé C, Grams AE, Stockhammer G, Kitzwoegerer M, Oberndorfer S, Marhold F, Weis S, Trenkler J, Buchroithner J, Pichler J, Haybaeck J, Krassnig S, Mahdy Ali K, von Campe G, Payer F, Sherif C, Preiser J, Hauser T, Winkler PA, Kleindienst W, Würtz F, Brandner-Kokalj T, Stultschnig M, Schweiger S, Dieckmann K, Preusser M, Langs G, Baumann B, Knosp E, Widhalm G, Marosi C, Hainfellner JA,
- Woehrer A, Bock C. The DNA methylation landscape of glioblastoma disease progression shows extensive heterogeneity in time and space. Nat Med. 2018 Oct;24(10):1611-1624. doi: 10.1038/s41591-018-0156-x. Epub 2018 Aug 27.
- Suwala AK, Stichel D, Schrimpf D, Kloor M, Wefers AK, Reinhardt A, Maas SLN, Kratz CP, Schweizer L, Hasselblatt M, Snuderl M, Abedalthagafi MSJ, Abdullaev Z, Monoranu CM, Bergmann M, Pekrun A, Freyschlag C, Aronica E, Kramm CM, Hinz F, Sievers P, Korshunov A, Kool M, Pfister SM, Sturm D, Jones DTW, Wick W, Unterberg A, Hartmann C, Dodgshun A, Tabori U, Wesseling P, Sahm F, von Deimling A, Reuss DE. Primary mismatch repair deficient IDH-mutant astrocytoma (PMMRDIA) is a distinct type with a poor prognosis. Acta Neuropathol. 2020 Nov 20. doi:10.1007/s00401-020-02243-6. Epub ahead of print.
- Keric N, Kalasauskas D, Freyschlag CF, Gempt J, Misch M, Poplawski A, Lange N, Ayyad A, Thomé C, Vajkoczy P, Meyer B, Ringel F. Impact of postoperative radiotherapy on recurrence of primary intracranial atypical meningiomas. J Neurooncol. 2020 Jan;146(2):347-355. doi: 10.1007/s11060-019-03382-x. Epub 2020 Jan 3.
Spine Surgery, Spinal Regeneration and Biomechanics
- Mern DS, Walsen T, Beierfuß A, Thomé C. Animal models of regenerative medicine for biological treatment approaches of degenerative disc diseases. Exp Biol Med (Maywood). 2020 Nov 11:1535370220969123. doi: 10.1177/1535370220969123. Epub ahead of print.
- Hartmann S, Thomé C, Abramovic A, Lener S, Schmoelz W, Koller J, Koller H.: The Effect of Rod Pattern, Outrigger, and Multiple Screw-Rod Constructs for Surgical Stabilization of the 3-Column Destabilized Cervical Spine – A Biomechanical Analysis and Introduction of a Novel Technique. Neurospine. 2020 Sep;17(3):610-629. doi: 10.14245/ns.2040436.218. Epub 2020 Sep 30.
- Wutte C, Becker J, Klein B, Mach O, Panzer S, Stuby FM, Strowitzki M, Maier D, Thomé C, Grassner L.: Early Decompression (<8 Hours) Improves Functional Bladder Outcome and Mobility After Traumatic Thoracic Spinal Cord Injury. World Neurosurg. 2020 Feb;134:e847-e854. doi: 10.1016/j.wneu.2019.11.015. Epub 2019 Nov 9.
- Petr, Ondra; Glodny, Bernhard; Brawanski, Konstantin; Kerschbaumer, Johannes; Freyschlag, Christian; Pinggera, Daniel; Rehwald, Rafael; Hartmann, Sebastian; Ortler, Martin; Thome, Claudius: Immediate Versus Delayed Surgical Treatment of Lumbar Disc Herniation for Acute Motor Deficits The Impact of Surgical Timing on Functional Outcome. SPINE. 2019; 44(7); 454-463.
- Beierfuß, Anja; Hunjadi, Monika; Ritsch, Andreas; Kremser, Christian; Thomé, Claudius; Mern, Demissew Shenegelegn: APOE-knockout in rabbits causes loss of cells in nucleus pulposus and enhances the levels of inflammatory catabolic cytokines damaging the intervertebral disc matrix. PLOS ONE. 2019; 14(11); e0225527. doi: 10.1371/journal.pone.0225527
- Warner, Freda M.; Jutzeler, Catherine R.; Cragg, Jacquelyn J.; Tong, Bobo; Grassner, Lukas; Bradke, Frank; Geisler, Fred; Kramer, John K.: The Effect of Non-Gabapentinoid Anticonvulsants on Sensorimotor Recovery After Human Spinal Cord Injury. CNS DRUGS. 2019; 33(5); 503-511. doi: 10.1007/s40263-019-00622-6
- Lener S, Wipplinger C, Stocsits A, Hartmann S, Hofer A, Thomé C. Early surgery may lower mortality in patients suffering from severe spinal infection. Acta Neurochir (Wien). 2020 Nov;162(11):2887-2894. doi:10.1007/s00701-020-04507-2. Epub 2020 Jul 29.
Functional Neurosurgery and Pain Therapy
- Frischer, Josa M.; Gruber, Elise; Schoeffmann, Verena; Ertl, Adolf; Hoeftberger, Romana; Mallouhi, Ammar; Wolfsberger, Stefan; Arnoldner, Christoph; Eisner, Wilhelm; Knosp, Engelbert; Kitz, Klaus; Gatterbauer, Brigitte: Long-term outcome after Gamma Knife radiosurgery for acoustic neuroma of all Koos grades: a single-center study.JOURNAL OF NEUROSURGERY. 2019; 130(2); 388-397.
- Reich, Martin M.; Horn, Andreas; Lange, Florian; Roothans, Jonas; Paschen, Steffen; Runge, Joachim; Wodarg, Fritz; Pozzi, Nicolo G.; Witt, Karsten; Nickl, Robert C.; Soussand, Louis; Ewert, Siobhan; Maltese, Virgina; Wittstock, Matthias; Schneider, Gerd-Helge; Coenen, Volker; Mahlknecht, Philipp; Poewe, Werner; Eisner, Wilhelm; Helmers, Ann-Kristin; Matthies, Cordula; Sturm, Volker; Isaias, Ioannis U.; Krauss, Joachim K.; Kuehn, Andrea A.; Deuschl, Guenther; Volkmann, Jens: Probabilistic mapping of the antidystonic effect of pallidal neurostimulation: a multicentre imaging study. 2019; 142(S); 1386-1398.
- Mahlknecht P, Peball M, Mair K, Werkmann M, Nocker M, Wolf E, Eisner W, Bajaj S, Quirbach S, Peralta C, Eschlböck S, Wenning GK, Willeit P, Seppi K, Poewe W.: Has Deep Brain Stimulation Changed the Very Long-Term Outcome of Parkinson’s Disease? A Controlled Longitudinal Study. Mov Disord Clin Pract.2020 Sep 21;7(7):782-787. doi: 10.1002/mdc3.13039.
Vascular Neurosurgery/ Neurointensive Care / Neurotrauma
- Chau, Charlene Y. C.; Craven, Claudia L.; Rubiano, Andres M.; Adams, Hadie; Tuelue, Selma; Czosnyka, Marek; Servadei, Franco; Ercole, Ari; Hutchinson, Peter J.; Kolias, Angelos G.: The Evolution of the Role of External Ventricular Drainage in Traumatic Brain Injury.JOURNAL OF CLINICAL MEDICINE. 2019; 8(9); 1422.
- Pinggera D, Steiger R, Bauer M, Kerschbaumer J, Luger M, Beer R, Rietzler A, Grams AE, Gizewski ER, Thomé C, Petr O. Cerebral Energy Status and Altered Metabolism in Early Severe TBI: First Results of a Prospective 31P-MRS Feasibility Study. Neurocrit Care. 2020 Jul 2. doi:10.1007/s12028-020-01042-x. Epub ahead of print.
- Ho WM, Görke AS, Glodny B, Oberacher H, Helbok R, Thomé C, Petr O. Time Course of Metabolomic Alterations in Cerebrospinal Fluid After Aneurysmal Subarachnoid Hemorrhage. Front Neurol. 2020 Jun 23;11:589. doi:10.3389/fneur.2020.00589.
- Petr O, Burrows AM, Brinjikji W, Brown RD, Lanzino G. Management of patients with an unruptured intracranial aneurysm and a history of malignancy. J Neurosurg Sci. 2020 Oct;64(5):413-419. doi: 10.23736/S0390-5616.17.04080-2. Epub 2017 May 31.
- Mayer L, Grams A, Freyschlag CF, Gummerer M, Knoflach M.: Management and prognosis of acute extracranial internal carotid artery occlusion. Ann Transl Med. 2020 Oct;8(19):1268. doi: 10.21037/atm-20-3169.
- Ho WM, Görke A, Petr O, Thomé C.: Treatment strategies of spinal arteriovenous fistulas and malformations: timing matters. J Neurosurg Sci. 2018 Apr;62(2):178-186. doi: 10.23736/S0390-5616.17.04260-6. Epub 2017 Nov 10.
- Patel B, Chatterjee A, Petr O, Collins H, Lanzino G, Derdeyn CP, Zipfel GJ.: T2-Weighted-Fluid-Attenuated Inversion Recovery Hyperintensity on Magnetic Resonance Imaging Is Associated With Aggressive Symptoms in Patients With Dural Arteriovenous Fistulas. Stroke. 2019 Sep;50(9):2565-2567. doi: 10.1161/STROKEAHA.118.024285. Epub 2019 Aug 14.
Selection of Funding
- AENEID – Academy for European Neurosurgical Excellence through Innovation and Diversity
- Erasmus+ program, European Union
- Several industry sponsored and academic clinical trials
Collaborations
- Charité Berlin, Berlin, Germany
- Charles University, Prague, Czech Republic
- Fondazione IRCCS Istituto Neurologico Carlo Italy Besta (FINCB), Milan, Italy
- Hopitaux Universitaire de Geneve, Geneva, Switzerland
- Hopitaux Universitaire de Montpellier, Montpellier, France
- Loma Linda University School of Medicine, Loma Linda, California, USA
- Mayo Clinic, Rochester, Minnesota, USA
- Muhimbili Complex, Dar es Salaam, Saudi Arabia
- Washington University School of Medicine, St. Louis,
- Weill Cornell Medicine, New York, USA