Anichstraße 35
6020 Innsbruck
Fax: +43 (0)50 504 22869
Email: Ute.Ganswindt@i-med.ac.at
Website: https://radioonkologie.tirol-kliniken.at/
Research year
Research Branch (ÖSTAT Classification)
104002, 106039, 106040, 210002, 301303, 301306, 301904, 302009, 302044, 302055, 302058, 302069, 302080, 302091, 303039, 303040, 304007, 305901, 102001, 102002, 102003, 102010, 102020, 102023, 103007, 103008, 103013, 103030, 202036, 202037, 206001
Keywords
Chemo-Immunotherapy, Dosimetry, Image guided radiotherapy (IGRT), Image processing, Oligometastases, patient reported outcomes, Radiation oncology, Radiation resistance, Radiosurgery, and Tumour cell biology
Research Focus
The delivery of high-precision radiotherapy (IMRT, IGRT and ART) is intended to yield enhanced oncological outcomes and a reduction in adverse effects. Prospective and retrospective observation of selected patient cohorts to optimize and personalize treatment decisions in the future. The clinical efficacy and biology of systemic medical treatments in combination with radiation therapy. The prediction of radiation resistance understanding biological processes and using multimodal imaging prior to, during and following treatment.
General Facts
The University Hospital for Radiation Oncology is the sole institution in its field in the entire province of Tyrol. Its mission is to provide the entire population of Tyrol with all available modalities of radiotherapy services. In 2024, the number of oncological patients treated exceeded 2000. The number of patients is increasing continuously at a rate of approximately 5-10% per year, a phenomenon that is primarily attributed to demographic shifts. In view of the high level of multidisciplinarity inherent in the treatment of cancer, radiation oncology constitutes a central component within the complex treatment schedules of tumour diseases. Radiation oncology represents a mandatory cross-sectional discipline, which is a prerequisite for participation in every multidisciplinary tumour board and Comprehensive Cancer Center (CCC).
The equipment comprises five linear accelerators, two brachytherapy units and one X-ray-device with a maximum output of 200 keV (e.g. for the treatment of benign diseases). Furthermore, a designated ward is established for the administration of systemic or supportive treatments.
It is notable that the majority of patients are in the outpatient setting concurrently. Consequently, the outpatient clinic is visited by more than 200 patients on a daily basis, which poses a significant logistical challenge.
The clinic is organised into four groups of medical doctors specialising in a defined group of tumour diseases or treatments. This ensures a high degree of specialised medical knowledge as well as a structured training for young doctors. The EXTRO-Lab is associated with the clinic and allows high level basic research in the field of radiation oncology.
In February 2025, a tenure-track position (§99/5) in the field of physics entitled “Image Guided Radiotherapy” was appointed (S. Kollotzek)
Biology “EXTRO-Lab”
Leader: Ira Ida Skvortsova
Marie Theres Eling (PhD student)
Sergej Skvortsov
The main objective is to investigate molecular properties of therapy-resistant and metastatically active carcinoma cells. A comprehensive elucidation of molecular pathways regulating metastatic spread and insensitivity to conventional therapeutic approaches has the potential to facilitate the developing potential biomarkers and new therapeutic targets. These, in turn, could assist in the prediction and improvement of unfavourable clinical outcomes in cancer patients. EXTRO-Lab is perfectly equipped to investigate the morphological and metabolic characteristics of cells, the capacities for cell invasiveness and motility, abilities for DNA repair and clonogenic survival after irradiation. Furthermore, the proteomic approach is used. Currently, we focus on breast cancer cells characterised by their ability to metastasise and to resist radiation.
Physics “Image Guided Radiotherapy”
Leader: Siegfried Kollotzek (Start February 2025)
The objective of the present research is twofold: firstly, to enhance the quality assurance (QA) of radiotherapy treatment, and secondly, to integrate dosiomics driven by artificial intelligence (AI) into research workflows. We focus on developing advanced QA methodologies, real-time treatment verification and radiation oncology feature extraction with the aim of improving treatment accuracy, outcome prediction and patient safety in image-guided radiotherapy (IGRT).
Research
With regard to the European landscape of radiation oncology institutions, the health system in Austria differs from that of many other countries. A mere 15 radiation oncology institutions are currently in operation, and they are all federally organised. Consequently, the delivery of radiotherapy services is predominantly undertaken by “high volume centres”, which facilitate the management of patient numbers and “stable cohorts” without the presence of significant selection biases. Furthermore, the organisation of long-term observation is less challenging in Austria than in many other European regions.
In 2018, the University Hospital for Radiation Oncology was restructured in terms of personnel resources and clinical research topics.
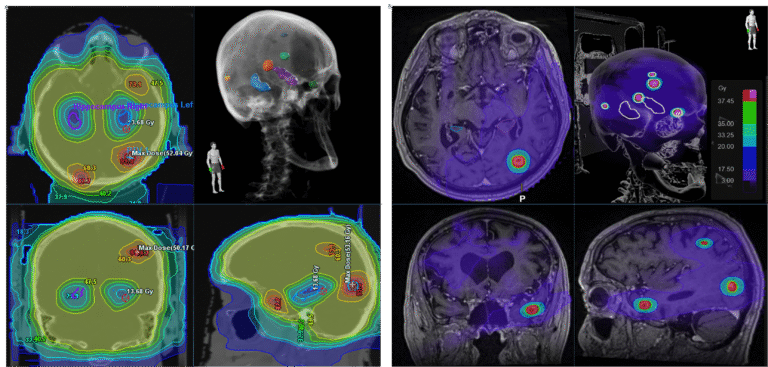
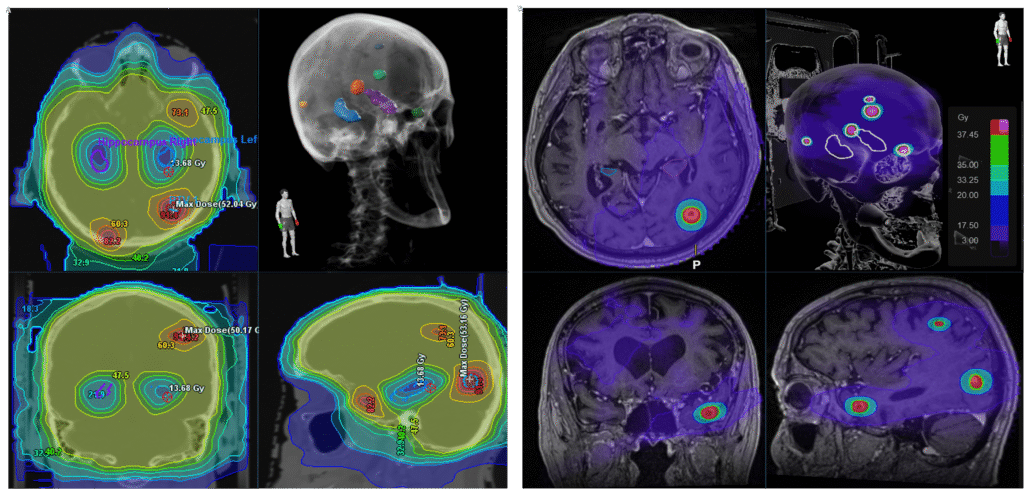
Neurooncology, Radiosurgery (J. Mangesius, M. Nevinny-Stickel, U. Ganswindt)
Retrospective analyses of treatment outcomes of large “Innsbruck” brain radiosurgery cohorts. Building data bases including systematic primary and secondary endpoints known from literature. Aiming to optimise radiosurgery fractionation schedules, radiosurgery techniques and supportive therapy approaches.
Prospective single-center trial (J. Mangesius): “Hippocampal Avoidance Whole Brain Radiotherapy (HA-WBRT) and Stereotactic Radiosurgery (SRS) in Patients with Multiple Brain Metastases – A Randomized Controlled Trial (HIPSTER)”. Including structured prospectively, neurocognitive testing in cooperation with MUI Psych 2 (M. Defrancesco) and neuroradiological analyses (MUI Neuroradiology – E. Gizewski, S. Mangesius). Recruitment of patients ongoing, first long-term results are awaited in 2025.
Breast Cancer (J. Mangesius, D. Minasch, T. Seppi, U. Ganswindt)
Aiming to analyse risk of radiation induced pneumonitis and the role of co-treatment with chemo-, endocrine and targeted therapy. Finalisation and publication of results of >400 patients in 2023 (s. publications below).
Oesophageal Cancer (J. Mangesius, K. Hörmandinger, U. Ganswindt)
Retrospective analyses of large South- and North-Tyrolean cohorts undergoing radiochemotherapy (definitive, neoadjuvant).
Image Guided Radiotherapy-IGDT (J. Mangesius, S.M. Vorbach, U. Ganswindt)
Intrafractional tracking in prostate cancer patients (s. publication below, worldwide 1st description of the method)
Stereoscopic X-ray, 3D surface imaging and cone beam CT for IGRT/SRS – cross modality evaluation (4-year PhD project R. Ibrahim, U. Ganswindt, S. Kollotzek, ongoing 2022-2026)
Stereotactic Treatment of Lung Metastases in Several Patient Cohorts (S.M. Vorbach, M. Nevinny-Stickel, U. Ganswindt)
Retrospective analyses of treatment outcomes of large “Innsbruck” lung radiosurgery cohorts. Building data bases including systematic primary and secondary endpoints known from literature. Aiming to optimise treatment decisions in common oligometastatic patients (s. publication below). Cooperations with comparable databases of other institutions and DEGRO AG Stereotaxie).
Implementation of Electronic Patient Reported Outcome Systems (S.M. Vorbach, M.P. Sarcletti, U. Ganswindt)
Cooperation with MUI Holzner et al. group. Using and programming CHES software for prostate and breast cancer patients, the most common solid tumours worldwide. Aiming to simplify and structure patient reported data sources to analyse outcomes, side effects and quality of life. Achieving “life-long electronic observation” of large patient group (incl. big data sources).
Biology “EXTRO-LAB”
Leader: Ira Ida Skvortsova
Marie Theres Eling (PhD student)
Sergej Skvortsov
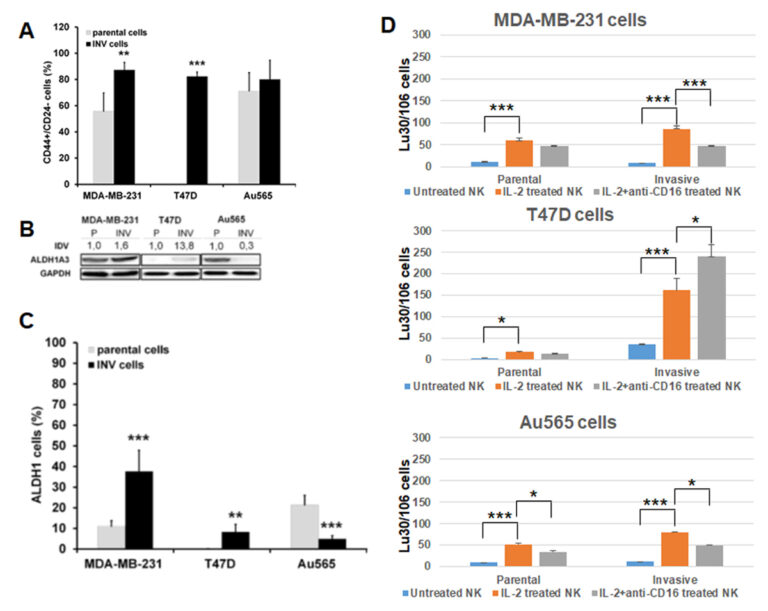
Current project (ongoing, unpublished): “Radiation-induced and obesity-dependent NK-cell sensitivities against metastatic breast cancer (BC) cells”:
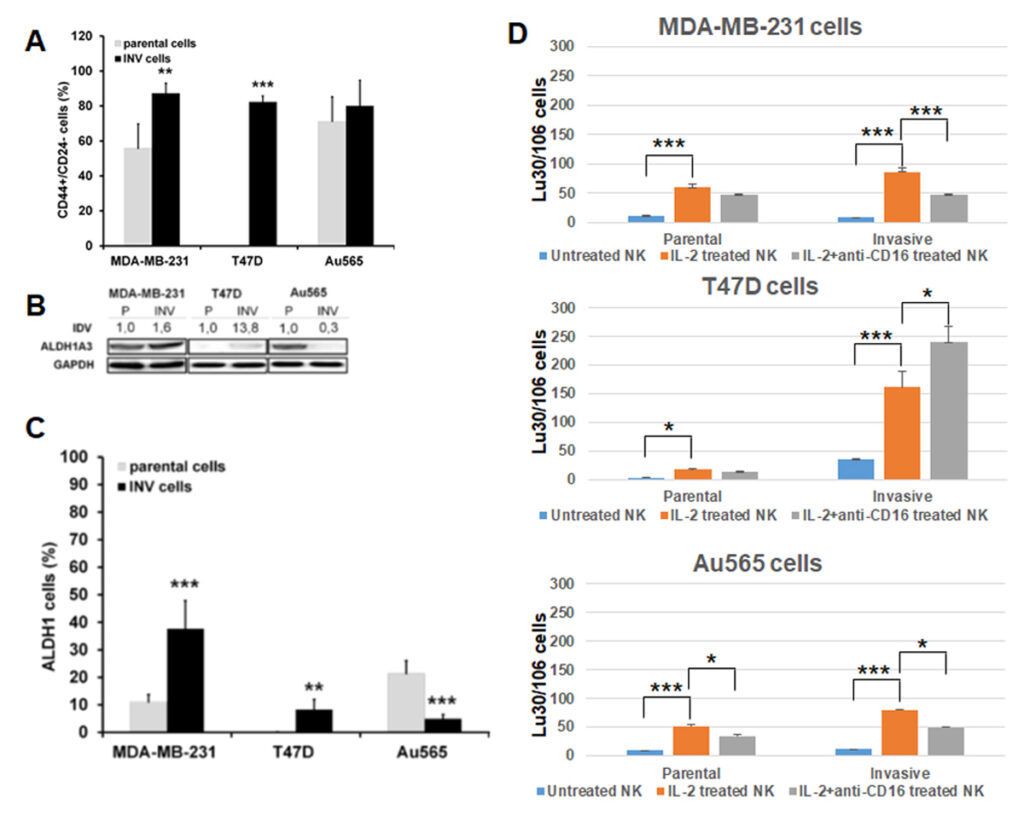
The primary objective of this study is to elucidate the role of an obese microenvironment in the regulation of cytotoxic activities of different doses of ionising radiation and NK cells against BC cells with enhanced metastatic properties. Metastasis cascade contains a number of steps such as cancer cell invasion in surrounding tissues followed by cell intravasation into the blood and/or lymphatic vessels, extravasation into the tissue of distant organs and, ultimately, the colonisation and growth in the targeted organs. We hypothesised that investigation of the molecular properties of BC cells with increased invasive abilities could provide a background for better understanding of radiation responses of metastatically active BC cells. Therefore, new in vitro models of BC cells with increased invasive potential were developed. The cells with enhanced invasive abilities (INV cells) were obtained from parental BC cells (MDA-MB-231 (triple-negative type (TNBC): oestrogen, progesterone and HER2/neu receptor-negative (ER-, PR-, HER2/neu-), T47D (luminal A type: ER+, PR+, HER2/neu-) and Au565 (Her2/neu-positive cells: ER-, PR-, HER2/neu+) after repetitive cell migration through the uncoated 8 µm-pore membrane in the Boyden chamber toward the cell culture medium containing an attractant (10% FCS). Since the enhancement of invasive and migratory abilities of BC cells can be closely associated with stemness properties, expressions of CD44+/CD24- and ALDH1 were evaluated in all parental and invasive BC counterparts (Figure 1A). It was found that INV BC cells exhibited an altered expression of cancer stem cell markers in comparison with their parental counterparts. (Figure 1B, 1C). We tested whether invasive BC cells are more susceptible to natural killer (NK) lysis than their parental counterparts (Figure 1D). While all INV cells exhibited an elevated sensitivity to NK lysis compared to their parental counterparts, T47D-INV cells demonstrated the most pronounced susceptibility to NK-dependent cell killing. It was therefore hypothesised that ER-positive BC could be more vulnerable to NK killing than other subtypes of BC cells.
Pictures
Selected Publications
Clinical Research:
- (•)Vorbach, SM, Sparano, F, Kreissl, S., Riedl, D., Sarcletti M.P., Ginestet, A., Holzner, B., Ganswindt, U., Lehmann, J.: Evaluating an electronic patient-reprted outcome monitoring system in patients with prostate cancer in routine clinical care: a prospective observational study. Qual Life Res. 2025 Apr 22. doi: 10.1007/s11136-025-03977-0. Online ahead of print. PMID: 40263189
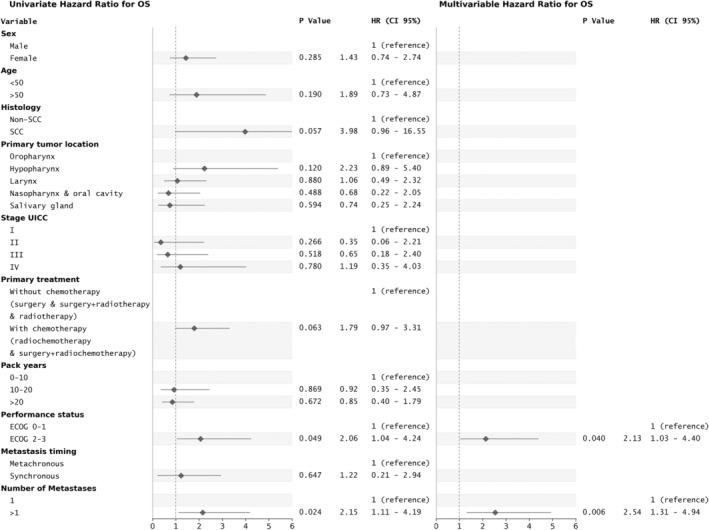
- (•)Vorbach, Samuel M.; Seppi, Thomas; Sarcletti, Manuel P.; Kollotzek, Siegfried; Mangesius, Julian; Lehmann, Jens; Riedl, David; Pointner, Martin J.; Santer, Matthias; Dejaco, Daniel; Nevinny-Stickel, Meinhard; Ganswindt, Ute: A novel prognostic score (HAMP) for head and neck cancer patients with single and multiple SBRT-treated lung metastases derived from retrospective analyses of survival outcome.
HEAD AND NECK-JOURNAL FOR THE SCIENCES AND SPECIALTIES OF THE HEAD AND NECK. 2025; 47(1); 242-253.
PubMed: 39114975 doi: 10.1002/hed.27913 [FLDID: 143459] IF: 2.400 (2023) / ZIT: 0 - (•)Mangesius, J.; Minasch, D.; Fink, K.; Nevinny-Stickel, M.; Lukas, P.; Ganswindt, U.; Seppi, T.: Systematic risk analysis of radiation pneumonitis in breast cancer: role of cotreatment with chemo-, endocrine, and targeted therapy.
STRAHLENTHERAPIE UND ONKOLOGIE. 2023; 199(1); 67-77.
PubMed: 36515701 doi: 10.1007/s00066-022-02032-y [FLDID: 140354] IF: 2.700 (2023) / ZIT: 8 - (•)Mangesius, Julian; Seppi, Thomas; Ibrahim, Ramine; Fleischmann, Katrin; Ginestet, Angela; Vorbach, Samuel; Hart, Tilmann; Pointner, Martin; Mangesius, Stephanie; Ganswindt, Ute: Dynamic intrafractional position monitoring with implanted fiducial markers for enhanced accuracy in radiotherapy of prostate cancer.
PHYSICAL AND ENGINEERING SCIENCES IN MEDICINE. 2023; 46(4); 1365-1374.
PubMed: 37523057 doi: 10.1007/s13246-023-01304-w [FLDID: 139805] IF: 2.400 (2023) / ZIT: 1 - (•)Mangesius, Julian; Seppi, Thomas; Arnold, Christoph Reinhold; Mangesius, Stephanie; Kerschbaumer, Johannes; Demetz, Matthias; Minasch, Danijela; Vorbach, Samuel Moritz; Sarcletti, Manuel; Lukas, Peter; Nevinny-Stickel, Meinhard; Ganswindt, Ute: Prognosis versus Actual Outcomes in Stereotactic Radiosurgery of Brain Metastases: Reliability of Common Prognostic Parameters and Indices.
CURRENT ONCOLOGY. 2024; 31(4); 1739-1751.
PubMed: 38668035 doi: 10.3390/curroncol31040132 [FLDID: 142362] IF: 2.800 (2023) / ZIT: 0
EXTRO-Lab:
- Federspiel, Julia, Steinbichler, Teresa Bernadette, Vorbach, Samuel Moritz, Eling, Marie Theres, Borena Wegene, Seifarth, Christof, Hofauer, Benedikt Gabriel, Dudas, Jozsef: Patient-Derived Cancer-Associated Fibroblasts Support the Colonization of Tumor Celss in Head and Neck Squamous Cell Carcinoma. Biomedicines. 2025 Feb 4;13(2):358. doi: 10.3390/biomedicines13020358. PMID: 40002772
- (•)Savic, Dragana; Steinbichler, Teresa Bernadette; Ingruber, Julia; Negro, Giulia; Aschenbrenner, Bertram; Riechelmann, Herbert; Ganswindt, Ute; Skvortsov, Sergej; Dudas, Jozsef; Skvortsova, Ira-Ida: Erk1/2-Dependent HNSCC Cell Susceptibility to Erastin-Induced Ferroptosis.
2023; 12(2); 336.
PubMed: 36672272 doi: 10.3390/cells12020336 [FLDID: 137383] IF: 5.100 (2023) / ZIT: 5 - Rauchenwald, Tina, Handle, Florian, Connoly, Catherine E., Degen, Antonia, Seifarth, Christof, Hermann, Martin, Tripp, Christoph H., Wilflingseder, Doris, Lobenwein, Susanne, Savic, Dragana, Pölzl, Leo, Morandi, Eva M., Wolfram, Dolores, Skvortsova, Ira-Ida, Stiotzner, Patrizia, Haybaeck, Johannes, Konschake, Marko, Pierer, Gerhard, Ploner, Christian: Preadipocytes in human granulation tissue: role in wound healing and response to macrophage polarization. Inflamm Regen. 2023 oct 31;43(1):53. doi: 10.1186/s41232-023-00302-5.PMID: 37904253
- zur Nedden, Stephanie; Safari, Motahareh S.; Weber, Dido; Kuenkel, Louisa; Garmsiri, Carolin; Lang, Luisa; Orset, Cyrille; Freret, Tom; Haelewyn, Benoit; Hotze, Madlen; Kwiatkowski, Marcel; Sarg, Bettina; Faserl, Klaus; Savic, Dragana; Skvortsova, Ira-Ida; Krogsdam, Anne; Carollo, Sandro; Trajanoski, Zlatko; Oberacher, Herbert; Zlotek, Dominik; Ostermaier, Florian; Cameron, Angus; Baier, Gottfried; Baier-Bitterlich, Gabriele: Protein kinase N1deficiency results in upregulation of cerebral energy metabolism and is highly protective in in vivo and in vitro stroke models.
METABOLISM-CLINICAL AND EXPERIMENTAL. 2024; 161; 156039.
PubMed: 39332493 doi: 10.1016/j.metabol.2024.156039 [FLDID: 143803] IF: 10.900 (2023) / ZIT: 0 - Su, Fengting; Descher, Hubert; Bui-Hoang, Minh; Stuppner, Hermann; Skvortsova, Ira; Rad, Ehsan Bonyadi; Ascher, Claudia; Weiss, Alexander; Rao, Zhigang; Hohloch, Stephan; Koeberle, Solveigh C.; Gust, Ronald; Koeberle, Andreas: Iron(III)-salophene catalyzes redox cycles that induce phospholipid peroxidation and deplete cancer cells of ferroptosis-protecting cofactors.
REDOX BIOLOGY. 2024; 75; 103257.
PubMed: 38955113doi: 10.1016/j.redox.2024.103257 [FLDID: 142496] IF: 10.700 (2023) / ZIT: 1
Selection of Funding
- FWF doc.fund Image-Guided Diagnosis and Therapy (IGDT), subproject 9: Stereoscopic X-ray, 3D surface imaging and cone beam CT for IGRT/SRS – cross modality evaluation: (U. Ganswindt)
- FWF I4140-B Glutamine metabolism as potential target for prostate cancer radiosensitization (S. Skvortsov)
- FWF P36528 Radiation-induced and obesity dependent NK-cell sensitivities against metastatic breast cancer cells (II Skvortsova)
Collaborations
- Grosu, S. Spohn, C. Zamboglou, University of Freiburg, Radiation Oncology, Germany
- Combs, J. Peeken, TU Munich, BZKF, “Leuchtturmprojekt AI”, Germany
- Rühle, University of Leipzig, Radiation Oncology, Germany – DEGRO AG Working Group Stereotaxie
- EORTC Quality of Life Group (Europe)
- AI Cluster, UKT Tübingen, Germany
- Bisio, Y. Ciribilli, CIBIO, University of Trento, Italy
- Kranjc-Brezar, M. Čemažar, G. Gašljević, Dept of Experimental Oncology, Institute of Oncology, Ljubljana, Slovenia
- Coer, University of Primorska, Faculty of Health Sciences, Izola, Slovenia
- Dubrovska, OncoRay – National Center for Radiation Research in Oncology, Dresden, Germany